A study by Drs. Ryan Walter, Donald Rinchuse, and Daniel Rinchuse shows a wide range of responses on the treatment of OSA
Abstract
Objective
The aim of this study was to survey orthodontists regarding the diagnosis, treatment, and outcomes of the treatment of obstructive sleep apnea (OSA).
Methods
An email invitation from the American Association of Orthodontists (AAO), AAO Partners in Education, was sent to a random sample of the members of the AAO in the United States and Canada (n = 2,300), requesting participation in a 13-question online survey (SurveyMonkey®) regarding the diagnosis, treatment, and outcomes of the treatment of obstructive sleep apnea (OSA).
[userloggedin]
A reminder email was sent approximately 2 weeks after the initial email. A total of 175 orthodontists participated in the survey.
[userloggedin]
 Results
Results
It was found that approximately 21% of the orthodontists that responded to the survey are carrying out some sort of sleep apnea therapy in their office. Of the doctors who treat sleep apnea, 42% initially attempt an oral appliance first with 7.9% combining this with a continuous positive airway pressure (CPAP) appliance.
According to our survey, approximately 13% of apnea cases being treated in orthodontic offices are receiving surgical intervention. The survey led to a number of differing responses when examining the types of diagnostic tools that are utilized to investigate reported cases of sleep apnea. Cephalometric analysis was the most commonly used radiographic examination, second only to clinical examination in diagnostic tools used. Cone beam computed tomography also was commonly used as a radiographic tool, with approximately the same diagnostic usage as photographic analysis. Diagnostic models were utilized only in approximately 29% of apnea cases in conjunction with other diagnostic tools. Concerning outcomes of those who treated sleep apnea, only slightly greater than 50% perceived their success rate in patient treatment to be greater than 50%.
Conclusions
This survey demonstrates that there is a great deal of variation in those treating sleep apnea, the methods with which they are diagnosing sleep apnea, and the outcomes of apnea treatment. Although many practitioners are referring out sleep apnea cases, according to the surveyed sample in our study, a significant percentage of orthodontists are treating this patient type. Further research and investigation into the optimal diagnostic tools, treatment types, and outcomes of treatment are needed.
Introduction
Obstructive sleep apnea (OSA) has been receiving a great deal of attention in the contemporary medical environment. Discussion about the condition has been increasing over the past 40 years. Estimates of the prevalence of obstructive sleep apnea have been variable, but the range can be fairly well estimated to be 2%-24%1,2,3 with most articles reporting somewhere around 8%1,2,3 of the U.S. population. The prevalence is estimated to be considerably higher in the male population3 as well as for those with higher body mass indices and excessive weight issues.4
The diagnosis and treatment of sleep apnea is a controversial topic in both the dental and orthodontic communities. Since this ailment is treated by both the medical as well as the dental community, there seems to be ambiguity regarding who should be the primary supervisor of treatment, how apnea should be evaluated, and what treatment should be pursued. Due to the fact that many treatment modalities for this disorder mirror, or are the same as, many procedures utilized in orthodontics,5-9 it is logical to assume that orthodontists should be considered to be among the primary team members in the diagnosis and management of OSA. Many of the intraoral devices used in the advancement of the mandible as a means of improving airway volume are essentially the same devices used in Class II orthodontic correction. Additionally, oral and maxillofacial surgeons have adapted the Bilateral Sagittal Split Osteotomy (BSSO) and Lefort I with maxillary advancement, commonly referred to as telegnathic surgery when utilized in correction of apnea, as two of the most common surgical interventions used in orthognathic surgical correction of this condition. Even if surgical intervention were attempted with the intention of correcting only a sleep apnea problem, a considerable probability exists that orthodontic intervention would also be recommended to establish favorable post-surgical occlusion. However, according to the literature, a lack of consistency exists regarding which specialists assume the roles of diagnostician and treating practitioner.
In addition to who should treat these patients and what role each should play in the treatment, there is a conflict about the diagnostic tools used to evaluate these patients. Sleep studies, including the polysomnogram (PSG), have been fairly well established as the gold standard of clinically evaluating sleep apnea.10-12 However, in their systematic review and meta-analysis of the medical literature, Ross, et al., found “this systematic review of the best available evidence for diagnosis of sleep apnea suggests that although numerous diagnostic strategies have been reported …There is some evidence in a relatively small number of patients, that should be expanded with more studies, suggesting that a full laboratory PSG may not be necessary to diagnose SA.”1 Most case studies on the subject in the orthodontic and dental literature and most papers concerning the topic of apnea suggest having a sleep observation evaluation on apnea patients.12 Although it would be difficult to justify any type of nonreversible type of intervention, including surgical intervention, without a proper sleep observation evaluation, it is conceivable that orthodontists may attempt reversible interventions such as passive oral appliances or continuous positive airway appliance (CPAP) appliance therapy to treat a portion of the population. Due to the high cost of PSG evaluation, the limited access to such evaluations in some areas, and many patients’ general resistance to undergo such testing, a percentage of the population will not receive a sleep study evaluation. Some researchers and practitioners have developed other instruments to evaluate potential apnea patients. Some claim that a clinical examination will discover many features, and this is important to the diagnosis of patients, particularly children.13
Additionally, cone beam computed tomography has been fairly well adopted as the best imaging modality to evaluate the airway.14,15 However, there also have been several proposed cephalometric analyses to examine the airway.16 Pracharktam, et al., found that cephalometric analysis could be utilized to identify apnea patients previously diagnosed through sleep study procedures (respiratory disturbance index >20).17 Shen, et al., more recently suggested several analyses of cephalometric measurements to evaluate obstructive sleep apnea.18 The proposed analyses utilized several commonly used landmarks, as well as several landmarks not commonly used in orthodontic practices, to help diagnosis apnea patients. Many practitioners utilize a combination of radiographic, photographic, and clinical evaluations to make an assessment before considering treatment of apnea patients.
In addition to the various forms of diagnosis of apnea patients, there are also several proposed treatment modalities for apnea, and many underscore the need for telegnathic surgical intervention with maxillary and/or mandibular advancement. Others are proponents of removable oral appliances utilized to advance the jaw and, thus, open the airway. Still others utilize a CPAP machine in the treatment of sleep apnea. Combinations of different therapies also are often used. The literature suggests a broad range of reported success in any given treatment modality, as well as an equally broad range regarding the stability of results.5-9
This discipline of dental sleep medicine includes a disparity of evidence-based findings and significant variance in diagnostic and management protocols. This study assesses the current trends in treatment of this disorder by surveying the treating population’s treatment modalities, diagnostic trends, results, and stability.
Materials and methods
A 13-question survey was sent to a randomized sample of orthodontists across the U.S. via email through the AAO. Orthodontic residents and faculty from a university orthodontic program worked concomitantly to develop the 13-question survey. After the development of the questionnaire, the survey was tested with the residents, and some of the language and grammar of a number of the questions was modified. The survey consisted of nine questions pertaining to sleep apnea treatment and four demographic questions.
A finalized copy of the 13-question survey was generated using SurveyMonkey. The survey was then passed along to the AAO for approval. One question was modified to include a write-in answer. A finalized survey tool was created using SurveyMonkey. The AAO then sent a link to the survey to a random sample of 2,300 orthodontists who were members of the AAO. The survey link was first sent on August 19, 2014. Surveys through the AAO are sent only to a portion of the population to minimize research emails to the group’s population. On September 1, a second email was sent to the surveyed population to increase participation. Collection of responses was closed on September 16 after a total of 175 responses. After data collection, the survey instrument was utilized to compile responses into useful figures and charts. Hand tabulation was also done using an Excel spreadsheet document.
Results
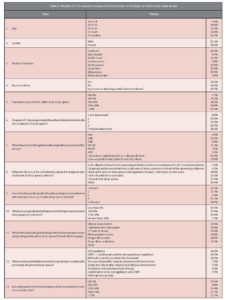
Of 2,300 emails sent to a random sample of orthodontists who are members of the AAO, 175 participated in the survey, amounting to a response rate of approximately 7.6%. The survey was completely anonymous. The important findings from the survey are shown in Table 1.
Approximately one-quarter of the responding survey participants are using some form of sleep apnea treatment in their offices with 35.5% believing that it is highly important for the orthodontist to be involved with treatment (4 or 5 on a 5-unit scale). Of those who treat sleep apnea, a significant portion treat only a very select segment of the presenting population — 42.3% treat less than 1% of those who present with sleep apnea, and 37.1% treat 1%-10% of the population of sleep apnea patients who present to their offices. Only 7.2% treated greater than 50% of the patients who presented to their office with OSA. In terms of diagnosis, 26.6% of the treating population of orthodontists attempted some intervention without completing a sleep study, 34.0% will not attempt any treatment at all without a sleep study analysis, and the remainder referred patients for sleep studies in certain cases, but not others that they treated. When analyzing the diagnostic tools used in evaluation of sleep apnea patients, 75% utilized a sleep study, 70% utilized a clinical exam, 58.8% utilized a cephalometric radiograph, 43.8% utilized computed tomography radiography, 43.8% utilized photographic records, and 28.8% utilized diagnostic models to aid evaluation. Some other tools listed were at-home sleep tests, soft tissue analysis, rhinomanometry, tomography, and neck size. When examining those who utilized cephalometric analysis, it was found that 22.1% of practitioners did not trace their cephalometric radiographs and, thus, had no particular angle that they utilized to evaluate airway. The angle between the sella-nasion and mandibular plane was most commonly used to evaluate the airway with 21.2% of practitioners finding this the most useful cephalometric angle to evaluate sleep apnea patients. SNB was the second-most utilized angle for this purpose with 20.4% of practitioners utilizing it. The remainder of the angles examined — SN-PP, AFH, SNA, and ANB — all showed less than 10% of practitioners finding these most useful. Of those treating sleep apnea, oral appliances are utilized as initial treatment in 34.2% of cases in this study, continuous positive airway pressure machines were used in 10.5% of patients, and 7.9% utilized a combination of these two treatments. Surgical intervention was utilized in 13.2% of patients with 7.9% having two-jaw telegnathic surgery, and 5.3% being treated solely with mandibular advancement. According to this survey, no patients were being treated with antidepressant therapy in orthodontic offices.
The perceived outcomes of those treating sleep apnea were as follows:
- 20.9% believed they had a success rate between 0%-5%.
- 8.8% believed they had a success rate between 5%-25%.
- 15.4% believed they had a success rate between 25%-50%.
- 27.5% believed they had a success rate between 50%-75%.
- An additional 27.5% believed their success to be greater than 75%.
A chi-square test examined the demographic data and the treatment questions. The examination revealed no correlation. This indicates that there was no change in treatment, diagnosis, and perception of outcomes due to region, gender, board certification, or age.
Discussion
The results of this survey demonstrate that a significant number of orthodontists are involved in the treatment of sleep apnea. However, as predicted, the diagnosis, treatments, assessment, and protocols surrounding the efforts of these treating practitioners are highly variable.
Many practitioners in this survey believe the prevalence of the condition to be much greater than it is generally reported in the literature.1-4 Approximately 50% (49.1%) of the orthodontists surveyed believed prevalence to be as high as 10% or greater, which according to much of the research, is fairly high.19 This perception may be due to the recent interest in this condition, which seems to be increasing over the past 10 to 20 years as more information is discovered about the condition. This interest has translated to an increasing number of articles, as well as dental involvement in the field.
In addition to the inflated perception of sleep apnea prevalence, a large portion of the orthodontic community who completed the survey believed that it was highly important for orthodontists to be involved in the treatment of sleep apnea patients — 35.5% scoring either a 4 or 5 on a scale of 1-5 for how important it was for orthodontists to be involved in treatment. With many of the treatment modalities of sleep apnea affecting occlusal relationships, it seems like a logical idea that the orthodontist should be involved in treatment of this ailment.6-9
The following aspects have yet to be established:
- Whether or not the orthodontist should be the primary treatment coordinator
- Who should initiate treatment
- Who should follow through with the course of treatment
- Who should follow up with the patient
If the orthodontist should simply evaluate for possible changes in occlusion and/or modify the occlusion to assist with treatment as someone else generally dictates the overall treatment plan
The orthodontist’s level of involvement currently will likely be dictated by the scope of the particular practice. While over one-third of respondents believe that the orthodontist should be involved in sleep apnea treatment, approximately one-quarter of orthodontists, 27.3%, believe that orthodontists’ involvement is of little or no importance in treatment of sleep apnea patients (a rating of 1 or 2 on the 5-point scale).  Since general dentists and oral surgeons also are trained in occlusion and capable of determining when occlusion may need to be modified, orthodontic cooperation may be redundant. However, treatment by an MD, e.g., a primary care physician, pulmonologist, ear, nose, and throat specialist, etc., may necessitate a greater involvement by orthodontists in order to give patients comprehensive medical and oral care.
Since general dentists and oral surgeons also are trained in occlusion and capable of determining when occlusion may need to be modified, orthodontic cooperation may be redundant. However, treatment by an MD, e.g., a primary care physician, pulmonologist, ear, nose, and throat specialist, etc., may necessitate a greater involvement by orthodontists in order to give patients comprehensive medical and oral care.
When considering the cephalometric evaluation orthodontists use for sleep apnea patients, there was no clear consensus as to which angles were most useful. However, SN-MP and SN-B were cited as most useful with 21.2% and 20.4% of the surveyed orthodontist population utilizing them respectively. Clearly, a high level of variability exists among those who use cephalometric measurements, as well as those who use cephalometric radiographs generally. In addition to the choices given, there were a large number of write-in responses as well as a significant portion of those who take cephalometric radiographs but do not trace them.
This study did, however, show that a number of orthodontists used cone beam computed tomography to analyze the airway. Although the research suggests that cephalometric radiographs can be effective in helping to analyze sleep apnea patients, current research suggests that cone beam computed tomography provides for a much better visualization tool.14,15 This raises the issue of clinicians’ need to expose these patients to minimal radiation. Most respondents support using CBCT scans for diagnosing sleep apnea patients; research agrees.14,15
Only approximately 20% of respondents perform any sort of sleep apnea therapy in their offices, which is interesting because most apnea treatment involves occlusal changes or, at the least, occlusal monitoring. Regarding referrals, most orthodontists refer to ear, nose, and throat specialists, oral surgeons, or pulmonologists in lieu of general dentists if further therapy apart from orthodontics is needed.
The term “diagnose” offers problems in this survey. In order to properly diagnose sleep apnea, clinicians need a sleep study.9,11 So many of our respondents were correct when they wrote responses that alluded to the necessity of sleep studies to properly diagnose sleep apnea. A more appropriate term perhaps would have been “evaluation” or “examination” for intended treatment. Perhaps some criticism is due in our profession for initiating therapy without a complete diagnosis. This survey clearly indicates that some practitioners fail to attain a full sleep study for each perceived obstructive sleep apnea patient. However, a substantial portion of the population would go untreated for this ailment if a full sleep study was required for every case. Also, some less severe apnea patients can be treated with noninvasive therapies without a sleep study diagnosis. A similar cursory diagnosis and treatment plan has been proposed and is currently used in the treatment of temporomandibular joint disorders.20 It is beyond the scope of this study to determine if this type of proposed treatment and diagnosis protocol is appropriate; however, perhaps orthodontists can research this further.
The survey demonstrates that orthodontic practitioners are using a variety of treatment modalities. With exception of antidepressant therapy, orthodontic practitioners are utilizing most mainstream treatments for sleep apnea today.6-9,21-25 Oral appliances are the number one treatment used by orthodontic practitioners. These appliances are fairly noninvasive and generally offer reversible effects, with the exception of some occlusal changes.24 In the authors’ opinion, this seems like acceptable treatment without a full diagnostic sleep study protocol, just as an occlusal guard may be used to alleviate idiopathic temporomandibular disorder. Additionally, it is not surprising that orthodontists often endorse surgery for sleep apnea patients. Although many of these patients may be treated solely for apnea, it is possible that some may need simultaneous correction of malocclusions. For example, a severely Class II patient with a retrognathic mandible and apnea would benefit from orthognathic advancement of his/her mandible. It is interesting that orthodontists recommend and use continuous positive airway pressure machines so readily. Training on how to utilize these machines is typically not part of the orthodontic or dental school curricula. The use of this device illustrates how popular the subject has become, and a substantial portion of the respondents have sought further training.
The respondents in this study illustrate a generalized interest in sleep apnea among orthodontists regardless of gender, age, board certification, or demographics. This issue is widespread, and interest is growing across all groupings within the dental profession.
This survey, of course, has some flaws, e.g., the small percentage of the total population surveyed (7.6%), which only scratches the surface of this topic. Clearly, further research is warranted.
Conclusions
This survey shows that orthodontists are involved in sleep apnea treatment and that controversy abounds regarding the evaluation and diagnostic criteria required for diagnosis and treatment. Additionally, it is clear that treatment outcomes are highly variable. Little consistency in any facet of sleep apnea treatment exists among the survey respondents. This is likely due to a lack of consensus and a lack of instruction about sleep apnea in dental schools and residency programs. A logical first step in creating uniformity in sleep apnea treatment within the dental profession is the augmentation and development of specific guidelines and curricula in dental schools for the orthodontic community.
The respondents in this survey demonstrated the following:
At least 20.7% of orthodontists who responded to the survey are currently carrying out some sleep apnea treatment.
Generally, orthodontists are neutral about their need to be involved in treatment (37.2% indicated a grade of neutral on a 5-point scale).
Generally, orthodontists believe the prevalence of sleep apnea is greater than reported in the literature.
Approximately 50% of respondents believe their treatment has a greater than a 50% success rate, and approximately 50% believe their treatment has a lower than 50% success rate.
Orthodontists are using variety of different tools to evaluate sleep apnea, including sleep studies, clinical examination CT scans, and cephalometric radiographs. Orthodontists use a variety of different therapies to treat sleep apnea, including oral appliance therapy, CPAP therapy, surgery, and combinations of these treatments. Many orthodontists do not treat sleep apnea and simply refer these patients to medical professionals for care.
There were no differences in treatment, examination, or perceived outcomes due to gender, age, location, or board-certification status.
There is a high level of variation within our profession concerning sleep apnea treatment, and further research and guidelines need to be established as a guide for orthodontists.
Acknowledgments
The authors of this article extend a special thank you to Drs. Charles Greene, Sanjivan Kandasamy, and John Stockstill for their assistance in the development of the survey.
View PDF For References: 44-48_Clinical Research-Walter
[/userloggedin]
[userloggedout][/userloggedout]
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


