CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This article aims to discuss the etiology of TMD, diagnosis criteria, and evidence-based management principles.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions with this quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Define some characteristics of TMD.
- Identify some guidelines for treatment of joint-related musculoskeletal disorders.
- Recognize some solutions for patients with inflammatory-orthopedic joint pain.
- Identify some characteristics of chronic myofascial pain.

Dr. Harold Menchel discusses the elusive nature of TMD
Abstract
Significant confusion and controversy still exist in the dental community about temporomandibular disorders (TMD). Because of this, dentists and orthodontists must be aware of some distinct etiologies when these patients present in their practices.
This article will review the etiology of TMD, the current diagnosis criteria for TMD (DC/TMD), and evidenced-based management principles. Since dentists often refer to orthodontists for TMD, it is essential that they can accurately diagnose these disorders and are able to manage orthodontic treatment in these patients according to these precepts.
Dentists will be able to quickly recognize simple from complex patients so that they know whom to treat and whom to refer. Two cases will be presented to illustrate these points.
Introduction
Misconceptions about TMD
Orthodontists are often referred TMD patients because the misconception that TMD is an “occlusal disease” is still pervasive in the dental community and in public perception. There is no support for this anachronistic belief1,2,3,4,5:
Mohlin B, et al., conducted a systematic review “to evaluate associations between different malocclusions, orthodontic treatment, and signs and symptoms of temporomandibular disorders (TMD).”6
Results included these findings:
- “TMD could not be correlated to any specific type of malocclusion.”
- “There was no support for the belief that orthodontic treatment may cause TMD.”
- “Associations between specific types of malocclusions and development of significant signs and symptoms of TMD could not be verified.”
Orthodontists, however, are still in an ideal position to diagnose and manage uncomplicated TMD cases. They are best prepared because of their skills with removable appliances and their knowledge and skills treating malocclusions that have been changed by TMD disorders, especially osteoarthritis. They need to acquire the diagnostic acumen to distinguish what they should treat and what they should refer and, in more complex cases, coordinate treatment with an orofacial pain dentist.
Facts about TMD
TMD is a medical musculoskeletal disorder involving two different populations of patients, although these populations can overlap. It is important that dentists focus on this when triaging TMD patients and not other distractions.
Some of these “distractions” are irrelevant occlusal considerations such as centric relation position, occlusal interferences, anterior guidance, and crossbites.7
There is also overemphasis on joint sounds in diagnosis of TMD. Painless clicking and popping is of no great concern if the patient has no locking. Painful clicking and popping associated with locking or joint crepitation are considerations, but these are easily determined and managed in most cases. Simple stethoscopic or digital examination is all that is required without other expensive instrumentation such as Doppler, which can produce false positives.8,9,10
By assuming TMD is mainly a disorder of muscles, and that chronic muscle pain is caused by overuse, dentists are often further distracted from the actual evidence base that this is mainly a disorder of joints. This will be discussed in detail.
Therefore, EMG measurements are not valid in diagnosing or managing TMD.11
The orthodontist has to recognize two distinct etiologies for TMD patients in order to manage these patients.
Population 1: Inflammatory-orthopedic joint pain
TMD disorders are no different from all other musculoskeletal orthopedic disorders. Therefore, the etiology, diagnosis, and management should follow established evidenced-based medical-surgical treatment guidelines. These guidelines are simple and well-established for any joint-related musculoskeletal disorder. There is no reason that the stomatognathic system should not be included along with all other body joints. These guidelines follow12,13:
- Control excessive forces on joints for both compression and hyperextension trauma
- Reduce inflammation (anti-inflammatory medications)
- Reduce muscle spasm (muscle relaxers)
- Mobilize the joint
In refractory cases (10% or less) more invasive approaches may be necessary — e.g., arthroscopic surgery. In terms of TMD, there are a minority of patients with disc displacement, and/or TMJ arthritis that may require surgery.
Population 2: Chronic myofascial pain
Thankfully, these patients are in the minority because they present diagnostic and management challenges for medical management. This population of patients often has widespread bilateral muscle pain and has generally poor prognosis.14,15
Comorbidities such as IBS, interstitial cystitis, chronic headache, anxiety, depression, chronic sleep disorders, restless leg syndrome, etc., are common. Fibromyalgia syndrome is an example.
These patients require a comprehensive team approach with medical and psychological management, and if they have a TMD component to their pain, an orofacial pain dentist. Most dentists should not get involved in primary management of these patients and should work closely with an orofacial pain dentist if patients require any dental treatment. Oral appliances are often ineffective. Occlusal treatment should be approached with utmost caution and should be avoided unless necessary. It is essential that the orthodontist be able to distinguish between these two different populations and avoid getting involved with the latter.
The diagnostic criteria for TMD
The first step for any dentist is to understand the diagnostic criteria first formulated in 199215,16,17 and then revised in 2010. These criteria divide TMDs into muscle and joint disorders (Table 1). The joint disorders are further divided into disc displacements and joint inflammatory disease. Combinations of these diagnoses are common.
A common misconception is that most TMDs are muscle disorders of common etiology. Actually, it is quite rare to find pain in the muscles of mastication without joint pain (Table 2). This belief is erroneously based in the unproven “neuromuscular” concepts that bruxism, occlusal interferences, and/or non-physiologic jaw position cause muscular hyperactivity leading to pain. Many dentists continue to believe this even today, although there is no support in the literature. There is even the mistaken belief that equilibration or occlusal therapy can eliminate bruxism.
In fact, muscle pain is of two types: the most common, joint mediated muscle pain (JMMP) related to population 1, and chronic myofascial pain (CMP) in population 2. The etiology of JMMP is well researched and documented while the mechanism for CMP is as yet unknown (Figure 1).
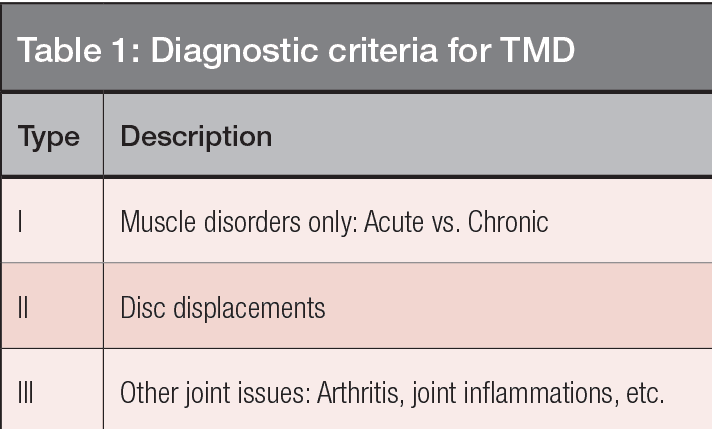
Table 1: TMDs are divided into three groups: disorders of muscle, disc displacements, and other joint disorders such as inflammatory joint disease (capsulitis-synovitis, osteo-arthritis). Source: Dworkin and Leresche 199215; Schiffman 201017
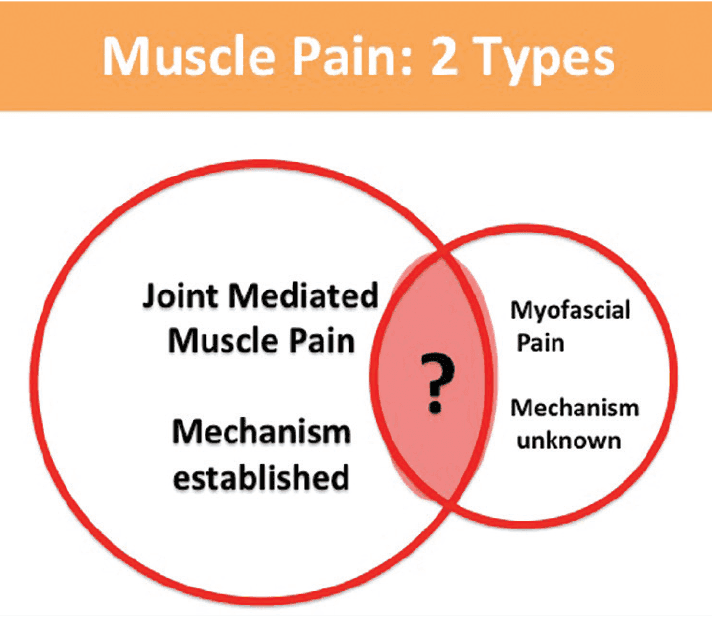
Figure 1: This Venn diagram illustrates the two populations of TMD-associated muscle pain. Most muscle pain is joint-referred with only a minority of cases with chronic myofascial pain (MP). The mechanism of MP is unknown at this time although the best evidence is that the pain is mediated by the central nervous system. Notice that the prevalence of just Type 1 muscle disorders is very low
Joint-mediated muscle pain
A basic principle of orthopedic medicine is that when a joint is painful or inflamed, this causes the muscles that move that joint to be painful and to spasm. This is known as “Hilton’s law” and has been taught in orthopedic programs since 1852.18
Patients who suffer from the most common musculoskeletal pain, lower back pain, are well aware of this.
In terms of TMD, most masseter and temporalis pain is joint mediated and can be alleviated by reducing joint pain and inflammation (Figure 3).
Treatment for an inflamed TMJ therefore follows basic orthopedic principles.
Remove load from the joint with rest, soft diet, behavioral modification, and flat plane full coverage bite splints when necessary, along with the principles previously listed.
Bruxism needs to be controlled and is a factor in TMD joint inflammation.19,20 This treatment is highly predictable and successful and is applicable to the majority of TMD patients that will present in an orthodontic practice.
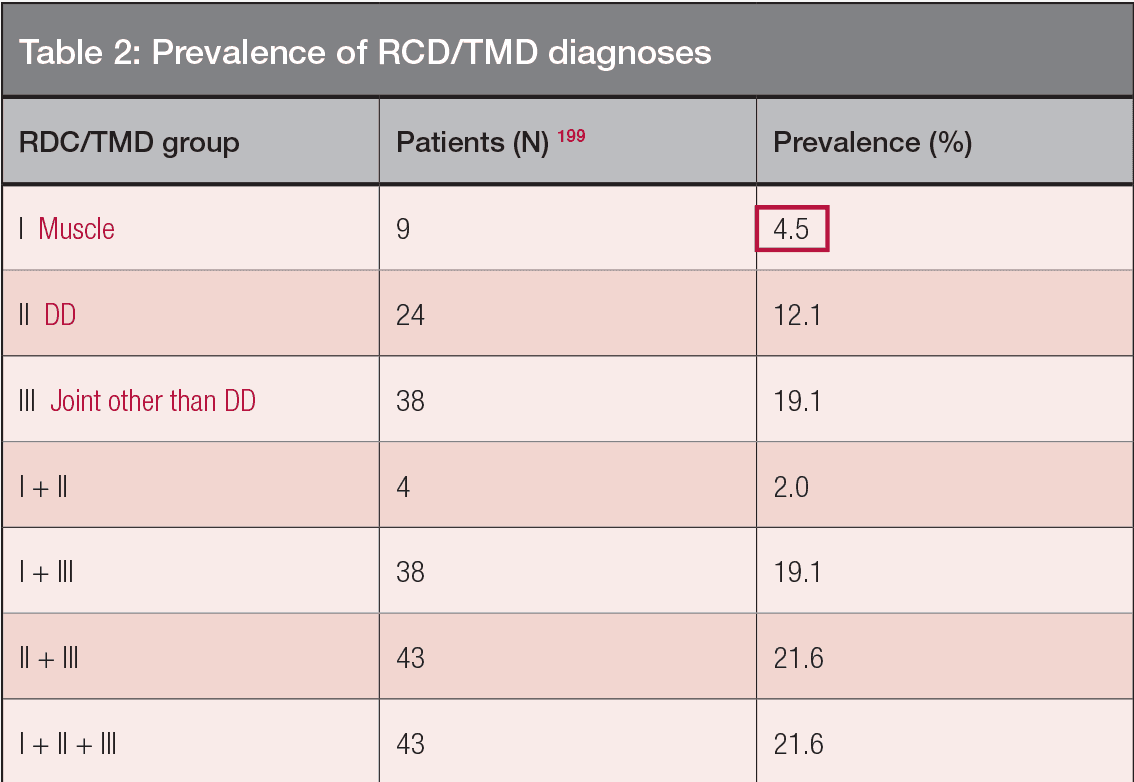
Table 2: Notice in this table that “pure” muscle pain (without joint pain) was only 4.5% of the sample. Although most of the sample had combined muscle and joint pain, it cannot be assumed that most of the muscle pain is joint mediated. With Permission from Danielle Manfredini
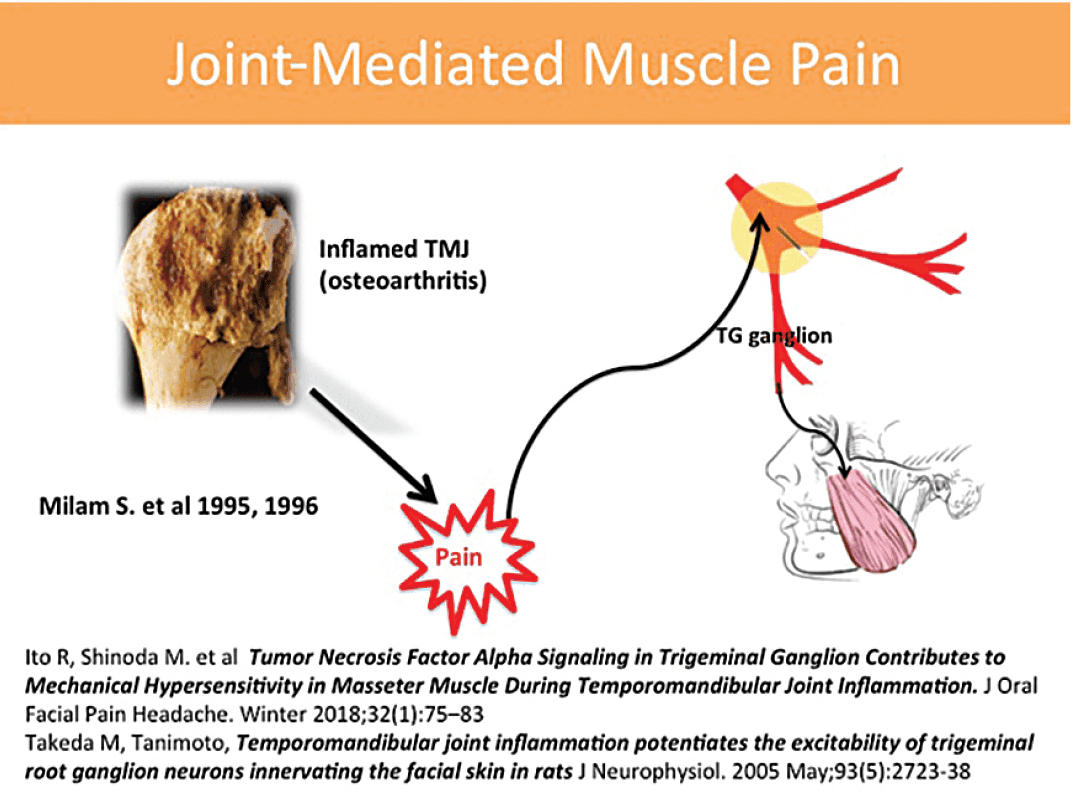
Figure 2: Joint-mediated muscle pain. The mechanism of most masseter muscle pain and spasm is referred and mediated through the trigeminal ganglion illustrated here. When joint pain and inflammation are reduced, the muscle symptoms follow along
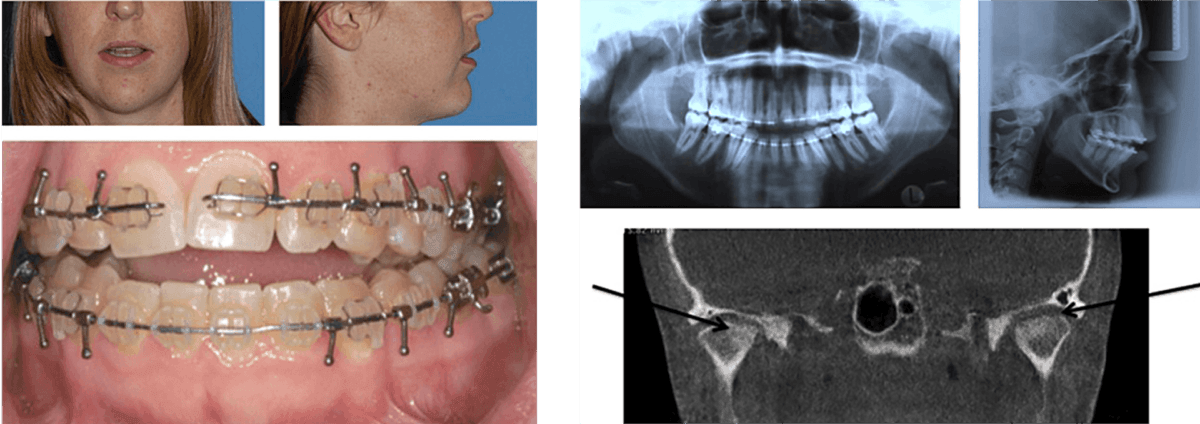
Figure 3: Case 1: TMJ osteoarthritis. 3A. Full lower face. 3B Profile. 3C. Initial presenta-tion with orthognathic appliances in place and Figure 4: Case 1: Imaging. 4A. Panorex 4B. Cephalometric film 4C. CBCT (note loss of cortical bone, flattening, and sclerosis of condyles in coronal view)
Chronic myofascial pain
The mechanism of chronic myofascial pain is unknown, although it is believed to be centrally mediated from CNS sensitization and biochemical changes.21,22 In most cases, it is not an overuse syndrome or related to excessive.23 These patients often have normal EMG activity. These patients have “knots” or trigger points in the muscles referring to other body parts. The exact mechanism of trigger point referral of pain is uncertain. Splints are often ineffective.24 Occlusal therapy should be avoided.
Conclusions
Orthodontists and dentists will succeed with basic conservative care with patients with joint pain and resultant muscle pain and myospasm. They should avoid treating patients with chronic widespread myofascial pain due to poor prognoses and refer these patients appropriately.
Case histories
Two cases are presented to illustrate the role of the orthodontist. In the first case, the patient has DC/TMD Type III osteoarthritis but also requires orthodontic-orthognathic surgery as result of her TMD. This is a case involving TMD joint pain and can be easily managed in an orthodontic practice so that the patient can proceed with dental treatment. It should be emphasized that her occlusal changes were related to ramus shortening and distal rotation of the mandible and are not a cause but a result of her TMD.
The second case is an illustration of a referral to an orthodontist of a patient with myofascial pain. This case should be referred. No occlusal therapy is indicated.
A previous article in Orthodontic Practice US, “Management of TMD during ortho-dontic treatment: disc displacements,”27 has discussed the management of disc displacements and patients with limited opening (DC/TMD) Type II.
Patient 1: Orthopedic-inflammatory diagnosis (TMJ osteoarthritis)
Subjective history
A 24-year-old female presents with history of TMJ pain and increasing anterior open bite. She had orthodontic treatment completed at age 14 and had relapse at age 17. She had orthodontics retreated but with relapse of the open bite. She was now treatment planned for orthognathic surgery.
Objective findings
The patient had severe pain to palpation of TMJ, masseter and moderate pain to temporalis palpation. The patient’s interincisal opening was limited to 34 mm (normal 45 mm – 55 mm). There was crepitation in both TMJs, and pain to loading was reduced with posterior placement of separator. The patient exhibited moderate wear with no tooth mobility. Her dental examination was otherwise unremarkable.
Imaging findings
Bilateral condylar loss of cortical bone, sclerosis, flattening, ramus shortening.
Diagnosis
- TMJ osteoarthritis with concomitant occlusal changes
- Protective myospasm (co-contraction)
Treatment
The appliances were removed, and an upper flat-plane orthotic inserted to be worn at night and as much as necessary during the day. The patient was prescribed meloxicam 15 mg QHS for 10 days and cyclobenzaprine 2.5-5 mg. QHS for 2 weeks
The patient was given instructions in soft diet, moist heat, and behavioral modification as necessary (no gum chewing, impact exercise).
Outcome
The patient’s pain was reduced 80% in 6 weeks with her opening normal at 50 mm.
Crepitation remains. She continues to wear the splint at night for evident bruxism.
She was also instructed to modify her diet permanently to avoid hard chewy foods or to ingest smaller chopped pieces. Her general dentist was informed to avoid extended mouth opening procedures for routine dentistry.
Orthodontics-orthognathic considerations
The patient cannot proceed to final bite correction without condylar and occlusal stability being established. She is also informed of risks and benefits of treatment in regard to possible relapse. Autoimmune inflammatory arthritis must be ruled out.
Protocol
For patients with bilateral degenerative joint disease, inflammatory arthritis must be ruled out. The standard of care in patients with inflammatory arthritis would be alloplastic (metal) joint replacements to establish stability.25
The protocol in this case follows:
- Referral to rheumatology for serology
- CBCT scan
- Follow patient on splint for 6-12 months of splint adjustment stability
- Final CBCT scan
Further studies, including nuclear medicine, MRI, etc., could be done but not chosen for this patient. This patient was followed for 12 months on her splint until there were minimal changes in the adjustment. A second CT was taken, which was diagnosed by the oral and maxillofacial radiologist as “stable arthritis”.26
Occlusal therapy
- Final leveling and aligning
- Lower bonded retainer with upper flat plane occlusal splint
Outcome
The patient has had stable occlusion 10-years postoperatively with minimal TMD and normal opening.

Figure 5: Case 1 postoperative. A. Panorex B. Cephalometric film C. Front facial D. Side facial E. Intraoral view
Discussion
Osteoarthritis is a common TMD diagnosis (25% of the patient presentation in my practice27). It is, of course, most predominant in older people but can present at any age. Osteoarthritis is a chronic disease with acute exacerbations as evidenced in Case 1. Once the inflammation is controlled, the joint, muscle pain, and spasm are alleviated. This is simple case to treat, well within the ability of all dentists in terms of pain and dysfunction. The important points here are that this patient had a joint disorder, which was treated with basic orthopedic principles. The patient has had no TMD for over 10 years even after the orthodontic-orthognathic surgery.
Patient 2: Chronic myofascial pain with referral
Subjective history
A 16-year old girl presented with a 1-year history of chronic headache.
She reports increased clenching and masseter fatigue. She was given an upper flat hard acrylic plane splint to be worn 24/7, which was well-made and adjusted. This was ineffective, and the patient reported that she felt it increased her clenching. She also was equilibrated by her dentist, which increased her symptoms.
She reported that her pain was least in the morning and increased as the day progressed. She had insomnia and fragmented sleep. Her opening was normal. She had finished orthodontic treatment at 13 with upper splint and lower labial bow retainer.
She recently saw another orthodontist who recommended retreatment. Tooth No. 15 was not completely erupted. Her medical history was significant for ADD, general anxiety, insomnia, and IBS. Her medications included Lexapro QHS, Adderall XR, alprazolam prn, and hyoscamine. She reported significant weight loss and was taking supplements to maintain weight. It was revealed that her symptoms were coincident with introduction of the stimulant because her school performance was poor. There was also a history of sexual abuse

Figure 6: Case history 2: Chronic myofascial pain. 6A. Intraoral presentation showing Angle Cl with minimal overjet and overbite, good alignment, minimal wear. 6B. Chart illustrating that the half-life of Ritalin is much less than Adderall XR and is less available during sleep to diminish bruxism
Objective findings
The patient had severe pain to palpation of the muscles of mastication, cervical muscles, and reported lower back pain. There were a number of trigger points in the masseter muscles referring pain to the teeth. She had minimal pain to TMJ palpation. Her imaging was normal. Her occlusion was within normal limits. She did not respond to joint loading or load testing. There was no wear on her teeth or on the splint
Diagnosis
- Chronic myofascial pain with referral
- Tension headache
Management
Much of the patient’s pain can be related to the introduction of the long-acting amphetamine, which has an elimination half-life of 11 hours. Management was focused on this, and with the coordination of her psychiatrist, the patient was changed to a short-acting methylphenidate (Ritalin) with a half-life of 2 hours only when she needed to focus and not on weekends. This was of great benefit and also improved sleep.
Because there was little evidence of nocturnal bruxism, the patient was given self-management techniques to control daytime bruxism, including classical conditioning with interval timer training to keep her teeth apart. She was also given trigger point injections, but the benefit was of short duration. Botox was considered but was not given due to the patient’s improvement.
Her headaches are reduced in frequency and controlled with OTC medications. She has an upper Essix retainer worn along with the lower labial bow retainer at night. The patient and her dentist were informed that any occlusal therapy was contraindicated.
Orders
- Referral to endocrinology for endocrine panel and thyroid panel (negative)
- Rheumatoid panel (negative)
- Cognitive behavioral therapy added to psychiatric treatment
Outcome
Overall the patient has 50% pain relief, improved coping skills, and improved sleep. Most importantly, she has come to realize that her headaches were not due to any “dental” or occlusal problems. There is no evidence of any bruxism.
Discussion
This patient, although in the minority of TMD patients, illustrates the continuing problem we have with dentists viewing TMD as an “occlusal disease.” Continuing education institutions that are sincere but have ignored the evidence base further promote this concept by focusing on occlusion. This occlusal concept has also led to situations where TMD patients are subjected to unnecessary dental treatment for their pain.
Conclusions
Orthodontists need to recognize that most TMD patients are orthopedic-inflammatory patients with joint pain etiology. These patients can be easily managed with basic medical principles by orthodontists. There also exist a minority of TMD patients with chronic myofascial pain who need to be referred for medical management. An oro-facial pain dentist is an ally to coordinate any dental treatment in TMD patients. Occlusion plays only a minor role in TMD.
References
- Gesch D, Bernhardt O, Kirbschus A. Association of malocclusion and functional occlusion with temporomandibular disorders (TMD) in adults: a systematic review of population-based studies. Quintessence Int. 2004;35(3):211-221.
- Rinchuse DJ. Does orthodontics cause TMJ disorders? Orthod Rev. 1987;1:11.
- Ash MM. Occlusions: reflections on science and clinical reality. J Prosthet Dent. 2003;90(4):373-384.
- Forssell H, Kalso E. Application of principles of evidence-based medicine to occlusal treatment of temporomandibular disorders: are there lessons to be learned? J Orofac Pain. 2004;18(1):9-22.
- Reynders RM. Orthodontics and temporomandibular disorders: a review of the literature (1966-1988). Am J Orthod Dentofacial Orthop. 1990;97(6):463-471.
- Mohlin B, Axelsson S, Paulin G, et al. TMD in relation to malocclusion and orthodontic treatment. Angle Orthod. 2007;77(3):542-545
- Clark G, Tsukiyama Y, Baba K, Watanabe T. Sixty-eight years of experimental occlusal interference studies: what have we learned? J Prosthet Dent. 1999;82(6):704-713.
- Mohl ND, McCall WD Jr, Lund JP, Plesh O. Devices for the diagnosis and treatment of temporomandibular disorders. Part I: Introduction, scientific evidence, and jaw tracking. J Prosthet Dent. 1990;63(2):198-201.
- Mohl ND, Lund JP, Widmer CS, McCall WD Jr.. Devices for the diagnosis and treatment of temporomandibular disorders. Part II: Electromyography and sonography. J Prosthet Dent. 1990;63(3):332-336.
- Mohl ND, Ohrbach RK, Crow HC, Gross AJ.Devices for the diagnosis and treatment of temporomandibular disorders. Part III: Thermography, ultrasound, electrical stimulation, and electromyographicbiofeedback. J Prosthet Dent. 1990;6(0):472-477.
- Henderson J. Orthopedic Principles: A Resident’s Guide. Ann R Coll Surg Engl. 2006;88(1):86-7.
- Raphael KG, Marbach JJ. Widespread pain and the effectiveness of oral splints in myofascial face pain. J Am Dent Assoc. 2001;132(3):305-316.
- Murray GM, Peck CC. Orofacial pain and jaw muscle activity: a new model. J Orofac Pain. 2007;21(4):263-278.
- Lim PF, Smith S, Bhalang K, De Slade GD, Maixner W. Development of temporomandibular disorders is associated with greater bodily pain experience. Clin J Pain. 2010;26(2):116-120.
- Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6(4):301-355.
- Dworkin SF, Huggins KH, Wilson L, et al. A randomized clinical trial using research diagnostic criteria for temporomandibular disorders-axis II to target clinic cases for a tailored self-care TMD treatment program. J Orofac Pain. 2002;16(1):48-63.
- Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Orofac Pain Headache. 2014;28(0):6-27.
- Hebert-Blouin MN, Tubbs RS, Carmichael SW, Spinner RJ. Hilton’s law revisited. Clin Anat. 2014;27(4):548-555.
- Raphael KG, Sirois DA, Janal MN, et al. Sleep bruxism and myofascial temporomandibular disorders: a laboratory-based polysomnographic investigation. J Am Dent Assoc. 2102;143(11):1223-1231.
- Türp JC, Komine F, Hugger A. Efficacy of stabilization splints for the management of patients with masticatory muscle pain: a qualitative systematic review. Clin Oral Investig. 2004;8(4):179-195.
- Milam SB, Schmitz JP. Molecular biology of temporomandibular joint disorders.J Oral and Maxillofac Surg. 1995;53(12):1448-1454.
- Milam SB, Zardentata G, Schmitz JB. Oxidative stress and degenerative temporomandibular joint disease: a proposed hypothesis. J Oral Maxillfac Surg. 1998;56(2):214-223.
- Sidebottom AJ. Alloplastic or autogenous reconstruction of the TMJ. J Oral Biol Craniofac Res. 2013;3(3):135-139.
- Bag AK, Gaddikeri S, Singhal A, et al. Imaging of the temporomandibular joint: An update. World J Radiol. 2014;6(8):567-582.
- Menchel H. Management of TMD during orthodontic treatment: disc displacements. Orthodontic Practice US. 2015;6(6):39-41.
- Krisjane Z, Urtane I, Krumina G, Neimane L, Ragovska I. The prevalence of TMJ osteoarthritis in asymptomatic patients with dentofacial deformities: a cone-beam CT study. Int J Oral and Maxillofac Surg. 41(6):690-695.
- Malki GA, Zawawi KH, Melis M, Hughes CV. Prevalence of bruxism in children receiving treatment for attention deficit hyperactivity disorder: a pilot study. J Clin Pediatr Dent. 2004;29(1):63-67.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Harold Menchel, DMD, is a dentist in Coral Springs, Florida, who limits his practice to TMD, orofacial pain, and sleep-disordered breathing. Dr. Menchel teaches undergraduate and graduate education in TMD and orofacial pain at Nova Southeastern School of Dental Medicine in Ft. Lauderdale, Florida. He is the director of orofacial pain at Larkin Teaching Hospital in Miami and lectures both nationally and internationally. Dr. Menchel is a fellow of the American Academy of Orofacial Pain, a Diplomate of the American Board of Orofacial Pain, and a member of the American Academy of Dental Sleep Medicine.
Harold Menchel, DMD, is a dentist in Coral Springs, Florida, who limits his practice to TMD, orofacial pain, and sleep-disordered breathing. Dr. Menchel teaches undergraduate and graduate education in TMD and orofacial pain at Nova Southeastern School of Dental Medicine in Ft. Lauderdale, Florida. He is the director of orofacial pain at Larkin Teaching Hospital in Miami and lectures both nationally and internationally. Dr. Menchel is a fellow of the American Academy of Orofacial Pain, a Diplomate of the American Board of Orofacial Pain, and a member of the American Academy of Dental Sleep Medicine.
