CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
The purpose of this article to discuss how combining technologies allows orthodontists choices when offering patients an alternative to extractions, implants, and orthognathic surgery.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions with the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify the characteristics of transposition.
- Identify some transposed teeth treatment options.
- Identify some benefits of TADs use.
- Realize some new technologies to aid in the timely completion of orthodontic treatment.

Dr. David Alpan discusses alternatives to extractions, implants, and orthognathic surgery
Abstract
Treating transposed teeth is very similar to impacted teeth or ectopic teeth. A detailed biomechanical plan is required to direct orthodontic forces to create the most ideal outcome, while minimizing unwanted effects. Utilizing temporary skeletal anchorage can allow forces to be unilaterally directed to improve orthodontic efficiency, and eliminating reciprocal forces that create unwanted movements of adjacent teeth. Incorporating accelerated orthodontics with micro-osteoperforations (MOPs) or pulsatile forces can facilitate difficult tooth movements in a reasonable treatment time, while increasing predictability and reducing negative sequela. Combining technologies allows ortho-dontists choices when offering patients an alternative to extractions, implants, and orthognathic surgery.
Introduction
Tooth transposition is defined as a reversal of the position with adjacent teeth in the same quadrant, particularly at the roots.4 Transposition may be incomplete when the crowns overlap, but the root apices are in their relative normal position, or complete when both the crowns and roots are parallel in their transposed malposition.1,2 Transposition is a form of ectopic eruption where one permanent tooth has interchanged its location in the dental arch, and it is not gender-specific.3 It is considered a rare dental anomaly, yet transposition has never been reported in both arches simultaneously nor in the deciduous dentition.4 The maxillary cuspid transposition is the most common, but it can happen in the mandibular arch as well.4
Transposed teeth treatment options include alignment in their transposed position, extraction of transposed teeth, extraction and replacement with implant(s), and orthodontic alignment to their normal position in the arch.1 Incorporating accelerated orthodontics (AO) with temporary anchorage devices (TADs) can significantly improve treatment outcomes when treating incomplete or complete transposed teeth into their normal position. Ideal treatment for trans-position would be prevention with early treatment to help guide the erupting teeth into the correct position in the arch. Early adolescent expansion and early extraction of deciduous teeth have shown to prevent transposition of teeth.5 People with transposed teeth do have some common traits such as congenital absence of teeth, peg-shaped lateral incisors, and severe arch-length discrepancies, which is the main etiology.6
Although the principle of orthodontic anchorage has been understood since the 17th century,7 it was not clearly defined until 1923 when Dr. Louis Ottofy8 defined it as “the base against which orthodontic force or reaction of orthodontic force is applied.” Most recently, Dr. John Daskalogiannakis9 defined anchorage as “resistance to unwanted tooth movement.” Fixed anchorage has played a significant role as an adjunct to orthodontic treatment in the last 2 decades. Mini plates and mini screws have been utilized in oral and maxillofacial surgery procedures for short- and long-term stability of bone fractures as well as orthognathic surgery for nearly 4 decades. Incorporating skeletal anchorage utilizing TADs, mini-screws, or mini plates as Drs. Jason B. Cope10 and John W. Graham11 had introduced over a decade ago, has impacted treatment outcomes, reducing the need for orthognathic surgery (Figures 1 and 2).

Figure 1: AY ceph initial skeletal Class III before treatment
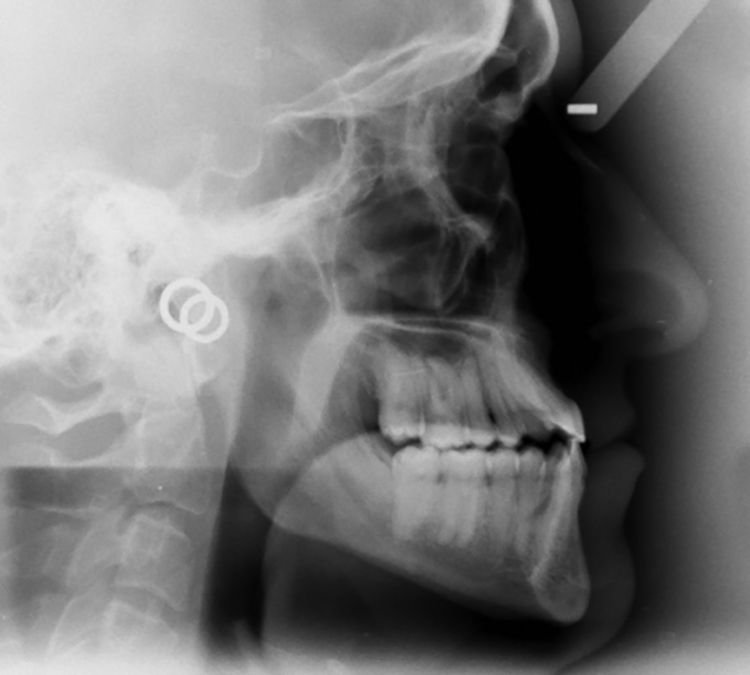
Figure 2: AY ceph after Invisalign® with TADs and AcceleDent® and TADs
Orthodontic biomechanics is all about juggling Newton’s third law of motion, defined as every action having an equal and opposite reaction. When applying forces to teeth, there is always a consideration that other teeth will move in an unwanted position. The introduction of TADs and mini-plates has given orthodontists the ability to reduce or eliminate the opposite reactive force.3 Utilizing skeletal anchorage allows orthodontists to move teeth in one direction, and the equal and opposite force is transferred to the bone that is fixed and has a large surface area to absorb the reactive force.3 TADs provide excellent anchorage to accomplish treatment goals otherwise needing orthognathic surgery, extractions, or implants. AO provides bone modulation affecting the biology of tooth movement on a cellular level.
Incorporating AO with the use of bone modulation technologies, such as vibration or micro-osteoperforation, has shown reduction in treatment time and increased treatment predictability.17,18,23,24,25 AO’s tangible benefits include decreased root resorption, decalcification, white spots, caries, gingivitis, periodontitis, loss of motivation, occlusal wear, and treatment time. These benefits are desired by the patients and practitioners alike.22 Early completion of treatment reduces chances of unwanted sequela and creates a more pleasant experience for the patient and practitioner.17 AO increases predictability and allows practitioners to treat more severe malocclusions in reasonable treatment times. Incorporating AO into practice requires alternative treatment planning, appointment intervals, and new practice management systems.19,20

Figure 3: Initial pano with large edentulous spaces

Figure 4: Final pano posttreatment with extractions PSL, TADs, and MOPs
Research and clinical outcomes
With the demands and expectations of the patients, orthodontists are motivated to reduce treatment time with AO and incorporate TADs to prevent more invasive procedures. Patients present with financial or emotional limitations around surgery and the possibility of, for example, retracting the mandibular arch to correct a skeletal Class III, which without surgery was unimaginable prior to TADs.3 (Figures 5 and 6)
Given the recent advances in biology, materials, and clinical treatment, this ortho-dontic tooth movement is not only a possibility, but also a reality.3 Clinicians’ daily dilemmas are a wide variety of malocclusions, ethnicities, sizes of teeth, variable bone biology, and various levels of patient compliance. Research demonstrates that accelerating the biology of tooth movement is a modality to add to our armamentarium.18,29,30,31,32
The practice of clinical orthodontics is managing the science of biomechanics, which inherently is harnessing or manipulating the biology of tooth movement.13,19 Treating transposition of teeth is a challenge diagnostically and therapeutically.12 Severe orthodontic malocclusions, such as complete transposition of teeth, are a difficult case type to demonstrate the utilization of TADs with AO to accomplish a normal tooth position in the arch (Figures 7-22).
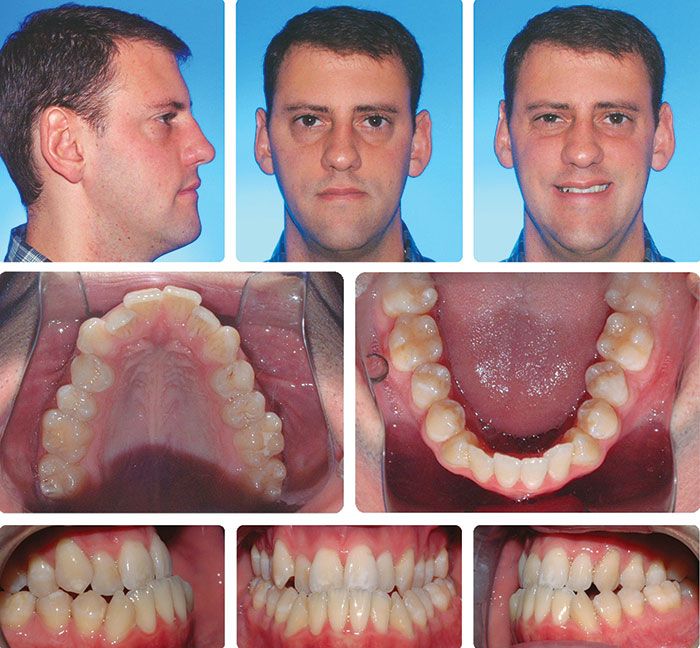
Figure 5: Before treatment skeletal and dental Class III with crowding and anterior crossbites

Figure 6: After treatment with PSL TADs in buccal shelf with NiTi springs — nonsurgical Class III correction
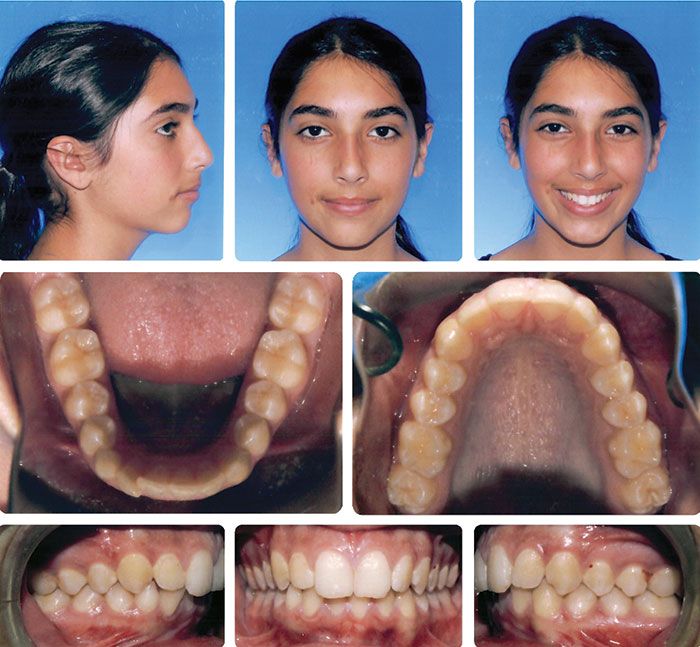
Figure 7: Initial pretreatment complete impaction and trans-position of mandibular right cuspid
Figure 8: Initial pano showing complete transposition of mandibular right cuspid
Figure 9: PA X-ray of impacted transposed cuspid bonded with a gold chain subgingival with primary closure
Figure 10: First TAD for skeletal anchorage; second TAD creating a pulley effect directing the force apical
Figure 11: Pulling the impacted transposed cuspid distal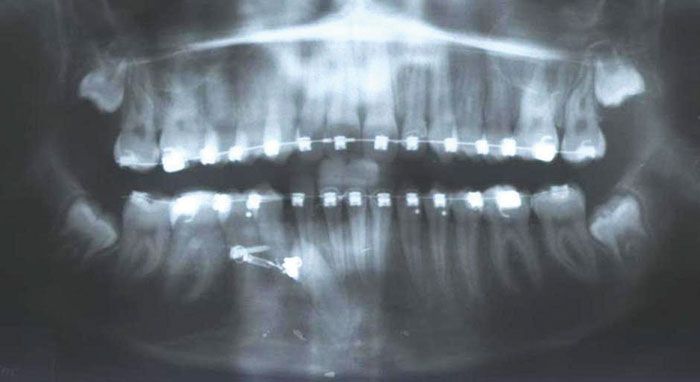
Figure 12: After crown in position removed one TAD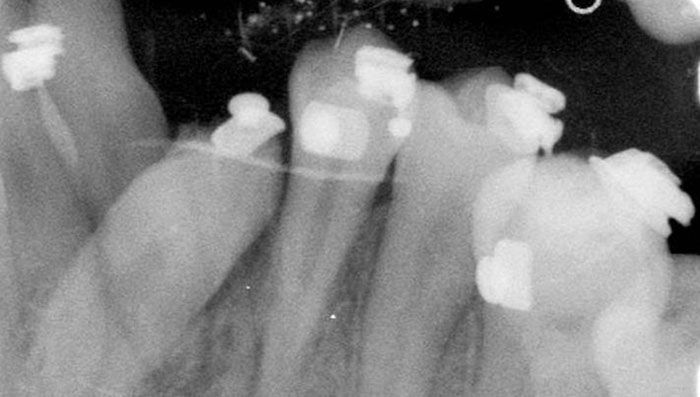
Figure 13: PA X-ray cuspid crown in place, root apex still transposed
Figure 14: Image of cuspid crown in cuspid position in arch, added a bracket with a power arm to help translate root apex
Figure 15: Progress using TAD with NiTi spring to power arm; started MOPs
Figure 16: Progress bi-dimensional forces; started vertical elastics and MOPs
Figure 17: Buccal TAD with NiTi spring for uprighting; lingual power chain keeping crown in lingual position
Figure 18: Crown and root in place 2 mm of attachment loss; removed TADs and springs; continue interarch elastics
Figure 19: Final images post TAD and MOPs procedure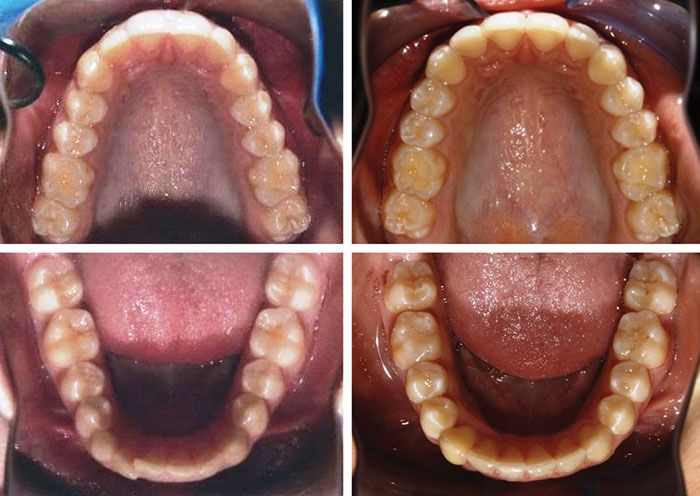
Figure 20: Initial and final occlusal images
Figure 21: Final pano with cuspid in normal position; mild root resorption of lateral incisor and cuspid
Figure 22: Performing MOPs with Propel
Case 1
The teenage female age 13 years 8 months (Figures 7-22) presented with a mandibular right cuspid in complete transposition with the mandibular right lateral incisor, which is a rare anomaly and not commonly seen.4 A similar situation presented several years prior, except on the left side, but I did not attempt to correct the transposition, and subsequently, there were heavy functional forces applied to the lateral incisor, which was not adequately structured morphologically to withstand those occlusal forces.
Figures 7-22 demonstrate an attempt to complete treatment with an ideal occlusal pattern with a full correction of an impacted transposed canine into its natural position in the arch. This treatment option would not have been possible if the impacted, transposed tooth was fully erupted. The root proximity and thin interdental bone limits this treatment option to only impacted transposed teeth that are not fully developed. The intrusion mechanics were performed subgingival similar to an impacted canine with primary closure post expose and bond. The initial intrusion mechanics presented in Figure 10 are applying one TAD with a NiTi closing spring with a twisted ligature wire slung as a pulley effect around the second TAD to direct the forces apically. Once the crown was intruded and tipped facially, I then distalized the cuspid with the first TAD with a NiTi spring; subsequently, the second TAD was removed as the crown was distalized into the arch. The patient utilized vertical elastics to extrude the mandibular right quadrant, as a remedy for the intrusion effect of all the adjacent teeth due to the extrusion of the mandibular right cuspid post distalization. Vertical, midline, Class II, and Class III elastics were prescribed to counteract all the forces required to achieve this result. The first TAD was used to help distalize the root with a TAD and a NiTi spring attached to a power arm on the bracket. Several bracket repositions were required to complete the uprighting and positioning of the cuspid back into the arch. Unfortunately, the patient did have some minor root resorption and recession requiring connective tissue grafting for the mandibular right cuspid.
Case 2
The young man (Figures 23-28) started as a Phase I treatment, and by his Phase II, he had developed an incomplete transposition of the maxillary left permanent cuspid in between the maxillary left central and lateral incisors. Phase I treatment consisted of maxillary 2 x 4 and mandibular lingual arch, no expanders. Since I had consolidated maxillary spaces from lateral to lateral in the Phase I, we were hoping the cuspid would follow the path of least resistance, but it did not and became impacted as an incomplete transposition. During his Phase II treatment, we intruded, distalized, and then extruded the maxillary left cuspid into the normal position within the arch.

Figure 23: Initial pano pre-phase I — cuspid position looks normal, but central and lateral incisor positions look abnormal

Figure 24: End of Phase I maxillary left cuspid erupting between the roots of the maxillary left central and lateral incisor. Notice the normal eruption of all the other teeth

Figure 25: Start of Phase II maxillary cuspid has erupted into the root of the maxillary left central
Figure 26: Initial Phase II ceph — cuspid is in a labial position in relation to the adjacent roots
Figure 27: Final pano with cuspid in normal position in the arch, with some resorption of the maxillary left central and lateral roots

Figure 28: Post Phase II maxillary left cuspid is no longer in a facial position but in the ideal position in the arch
MOPs technique is similar to TAD placement
In 1988 to 2010, multiple researchers found that the application of NSAIDs decreased the rate of tooth movement significantly, and cytokines played an important role in activating the bone-remodeling machinery.13,19,25 Removing all NSAIDs in combination with accelerating the biology of tooth movement via MOPs or with vibration is paramount. Research shows if inhibiting the expression of certain cytokines decreases the rate of tooth movement,7 then if we perform an iatrogenic trauma to stimulate the expression of inflammatory cytokines through small micro-osteoperforations (MOPs) (Figure 22) of the cortical bone, research shows MOPs increase the rate of bone remodeling and ultimately increase the rate of tooth movement.13 Previous studies have demonstrated that bone injury causes cytokine release and leads to an accelerated bone turnover and a decrease in regional bone density.14,15,16,17,20 The idea of traumatizing the bone is not novel and is now correlated with the increase in the inflammatory cytokines that can increase bone remodeling.18 I routinely perform this procedure as if I was placing a TAD or changing an archwire.
The MOPs technique is outlined and explained in the April 2016 article in Orthodontic Practice US.28 Some patients require the use of a local anesthetic via syringe, but in most cases, profound topical is sufficient. Mild discomfort is experienced by the patient postoperatively, usually for 24-48 hours, and is moderated with Tylenol® only, no NSAIDs.18,29,31,32 MOPs can be localized to two teeth whereas pulsatile forces affect all the teeth. When using MOPs, there is no issue of patient compliance as there is with vibration. MOPs are performed every 12-16 weeks depending on the patient’s treatment response. The depth of perforation is usually 3 mm-5 mm. Patients’ soft tissue can vary in thickness from 1 mm-2.5 mm in thickness. So, the tip will go into the cortical plate and microfracture the cortical bone about 1.5 mm-3 mm in depth, also referred to as alveolocentesis.
TADs can be located transosteally, subperiosteally, or endosteally; and they can be fixed to bone either mechanically (cortically stabilized) or biochemically (osseointegrated).3 I prefer the Vector TAD system and will use a 6 mm or 8 mm TAD based on the anatomy and position desired. The procedure is very similar to MOPs except the TAD is screwed in once and left in place. There is a huge concern for root proximity, thus PA X-rays are taken prior to placement and after for verification.3
Pulsatile forces or vibration technique
Since OrthoAccel® publicly launched AcceleDent® Aura in early 2012 and now Optima™ in 2017, clinicians and patients are experiencing reduction in treatment time,34,35,36 increased treatment predictability, and a pleasant analgesic effect.37 Micropulse vibration, 20 min/day at a frequency of 30 Hz at a force of 0.25N (25g) in combination with orthodontic treatment is demonstrating reduced treatment time or acceleration of tooth movement. The clinical research states a 50% increase in the rate of tooth movement,18,34,35,36 but I have found this does not correlate to the same reduction in overall treatment time. Acceleration is more efficient during leveling and aligning then sagital corrections.35 With AO, I am observing an average of 35% reduction in overall treatment time dependent on the appliance choice, mechanics utilized, or compliance with acceleration devices.
Pulsatile forces offer an analgesic effect,37 which MOPs do not. To be efficient and make AO work, treating orthodontists would have to change patients’ appointment intervals. Patients who choose vibration need to be compliant daily: I check the compliance interface at each visit, which gives a chronologic history by day, month, time, and length of use. For fixed braces, we are activating treatment every 3 weeks.
Practice management considerations
Informed consents for treating transposed teeth into their ideal position in the arch are highly recommended. The prognosis can be questionable based on the treatment plan and proximity of teeth to adjacent structures. Use of CBCT 3D digital records is strongly recommended as viewing the path of eruption will help with proper treatment planning with the ideal mechanics needed.12 Since there are risks involved such as root resorption, root damage, mobility, and loss of periodontal support, the patient must be informed in comparison to the benefits. Informed consents are signed by all patients who are undergoing AO, and separate informed consents for all patients being treated with TADs.
My initial application of MOPs is for difficult or stubborn teeth — e.g., impacted or transposed teeth, or laterals treated with aligners. Treatment acceptance with MOPs is higher with existing patients who need to get completed just based on their cost. We recommend AO to all extended treatments as we begin to see they will not meet their estimated treatment time. Wanting to finish treatment as soon as possible, patients toward the end of treatment find AcceleDent to be cost-prohibitive and are more receptive to MOPs. Fee considerations play a role in the doctors’ and patients’ decisions. Recently, patients have incorporated the AO into the total treatment fee, and I have found a higher case acceptance. I have also chosen a no-fee MOPs treatment, as there is a benefit to completing treatment early. (Extended treatment costs are greater than the cost of the Propel tip.)
Patients are able to reliably accelerate their treatment with a cost-effective, minimally invasive procedure such as MOPs32 or with low-frequency vibration. Some AO alternatives such as Wilckodontics® or Piezosurgery® are not cost-effective and require surgery at a price range of $5,000-$10,000.There is a potential for negative sequela and extended recovery time with these surgical procedures. AcceleDent may be more costly, but vibration requires no doctor chair time and is less clinical work. If the patient is not compliant, vibration has little to no clinical effect.
Orthodontic fee agreements are either paid in full or spread over time. The majority of orthodontists require the full fee due by treatment finish. Patients appreciate the convenience of paying the treatment over time, as it lowers their monthly fee. Since AO has changed the original estimated treatment time, we have had to update existing contracts. This poses a new challenge with our new starts, since we don’t have as much time to amortize their fee. For some patients, we have extended the payment arrangements past the finish date, but most patients are asked to complete payment by the end of their treatment. We have added this language to our contract to assist us with this issue: “If the active phase of treatment is completed before the agreed estimated time, the full fee is due and payable at that time.” The commitment needs to be agreed upon before AO treatment is initiated.
Conclusion
TADs with AO can facilitate treatment outcomes only seen with orthognathic surgery or extractions. Preventing transposition of teeth with early detection and early expansion treatment monitored with CBCT scans can help to prevent teeth from becoming transposed.5 Treating transposition of teeth can now be successfully managed with the use of CBCT imaging and progressive biomechanics utilizing TADs and AO. Incorporating AO with TADs can significantly improve treatment outcomes when treating incomplete or complete transposed teeth into their normal position. Orthodontists can now recommend alternative treatment plans that would have never been an option with traditional mechanics. The benefits of decreased treatment time and increased predictability far outweigh any of the costs or additional work required by the patient or the practitioner utilizing AO. TADs have proven to be an effective anchorage device to control or harness anchorage not available with just tooth-borne appliances. Combining PSL, TADs, and AO has allowed for more complicated treatment outcomes that were not even an option in the past.
References
- Shapira Y, Kuftinec MM, Stom D. Maxillary canine-lateral incisor transposition — orthodontic management. Am J Orthod Dentofacial Orthop. 1989;95(5):439-444.
- Joshi MR, Bhatt NA. Canine transposition. Oral Surg Oral Med Oral Pathol. 1971;31(1):49-54.
- Singh K, Kumar D, Jaiswal KR, Bansal A. Temporary anchorage devices — mini implants. Natl J Maxillofac Surg. 2010;1(1):30-34.
- Shapira Y, Kuftinec MM. Tooth transpositions — a review of the literature and treatment considerations. Angle Orthod. 1989;59(4):271-276.
- Trivedi BD. Early Diagnosis and prevention of complete transposition of mandibular lateral incisor during mixed dentition. Pediatr Dent Care. 2016;1(1):102
- Shapira Y, Kuftinec MM. Orthodontic management of mandibular canine-incisor transposition. Am J Orthod. 1983;83:271-276.
- Creekmore TD, Eklund MK. The possibility of skeletal anchorage. J Clin Orthod. 1983;17(4):266–269.
- Ottofy, L. Standard dental dictionary. Chicago, IL: Laird & Lee, Inc.; 1923.
- Daskalogiannakis J. Leipzig: Quintessence Publishing Co; 2000. Glossary of Orthodontic Terms
- Herman R, Cope J. Temporary anchorage devices in orthodontics: mini implants. Semin Orthod. 2005;11:32-39.
- Graham JW, Cope JB. Miniscrew Troubleshooting. Orthodontic Products. 2006;13(3):26-32
- Lee MY, Park JH, Jung JG, Chae JM. Forced eruption of a palatally impacted and transposed canine with a temporary skeletal anchorage device. Am J Orthod Dentofacial Orthop. 2017;151(6):1148-1158.
- Teixeira CC, Khoo E, Tran J, et al. Cytokine expression and accelerated tooth movement. J Dent Res. 2010; 89(10):1135-1141.
- Frost HM. The regional acceleratory phenomenon: a review. Henry Ford Hosp Med J. 1983;31(1):3-9.
- Frost HM. The biology of fracture healing. An overview for clinicians. Part I. Clin Orthop Relat Res. 1989;248:283-293.
- Frost HM. The biology of fracture healing. An overview for clinicians. Part II. Clin Orthop Relat Res. 1989;248:294-309.
- Shih MS, Norrdin RW. Regional acceleration of remodeling during healing of bone defects in beagles of various ages. Bone. 1985;6:3(5)377-379.
- Alikhani , Raptis M, Zoldan, et al. Effect of the micro-osteoperforations on the rate of tooth movement. Am J Orthod Dentofacial Orthop. 2013;144(5):639-648.
- Arias OR, Marquez-Orozco MC. Aspirin, acetaminophen, and ibuprofen: their effects on orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2006;130(3):364-370.
- Yaffe A, Fine N, Binderman I. Regional accelerated phenomenon in the mandible following mucoperiosteal flap surgery. J Periodontol. 1994;65(1):79-83.
- Adachi Y, Okazaki M, Ohno N, Yadomae T. Enhancement of cytokine production by macrophages stimulated with (1–>3)-beta-D-glucan, grifolan (GRN), isolated from Grifola frondosa. Biol Pharm Bull. 1994;17(12):1554-1560.
- Alhashimi N, Frithiof L, Brudvik P, Bakhiet M. Orthodontic movement Arend WP, Palmer G, Gabay C (2008). IL-1, IL-18, and IL-33 families of cytokines. Immunol Rev. 2000;223:20-38.
- Başaran G, Ozer T, Kaya FA, Hamamci O. Interleukins 2, 6, and 8 levels in human gingival sulcus during orthodontic treatment. Am J Orthod Dentofacial Orthop. 2000;130(1):e1-6.
- Dale DC, Boxer L, Liles WC. The phagocytes: neutrophils and monocytes. Blood. 2008;112(4):935-945.
- Alhashimi N, Frithiof L, Brudvik P, Bakhiet M. Orthodontic movement induces high numbers of cells expressing IFN-gamma at mRNA and protein levels. J Interferon Cytokine Res. 2000;20:7–12.
- Dienz O, Rincon M. The effects of IL-6 on CD4 T cell responses. Clin Immunol. 2009;130(1):27-33.
- Krishnan V, Davidovitch Z. On a path to unfolding the biological mechanisms of orthodontic tooth movement. J Dent Res. 2009;88(7):597-608.
- Nicozisis J. Accelerated orthodontics through micro-osteoperforation. Orthodontic Practice US. 2013;4(3):56-57.
- Guinn K. Propel orthodontics enabling faster and more predictable results. Orthotown magazine. December 2013;38-41.
- Pobanz J, Storino S, Nicozisis J. Orthodontic acceleration: Propel alveolar micro-osteoperforation. Orthotown magazine. May 2013;1-4.
- Nicozisis J. Accelerated tooth movement technology. Orthotown magazine. July/Aug 2013;1-4.
- Garlet TP, Coelho U, Silva JS, Garlet GP. Cytokine expression pattern in compression and tension sides of the periodontal ligament during orthodontic tooth movement in humans. Eur J Oral Sci. 2007;115(5):355-362.
- Uribe F, Padala S, Allaredidy V, Nanda R. Patients’, parents’, and orthodontists’ perceptions of the need for and costs of additional procedures to reduce treatment time. Am J Orthod Dentofacial Orthop. 2014;145(suppl 4)65-73.
- Pavlin D, Anthony R, Raj V, Gakunga PT. Cyclic loading (vibration) accelerates tooth movement in orthodontic patients: A double-blind, randomized controlled trial. Seminars in Orthodontics. 2015; 21(3): 187-194.
- Bowman SJ. The effect of vibration on the rate of leveling and alignment. J Clin Orthod. 2014; 48(11):678-688.
- Ortan-Gibbs S, Kim NY. Clinical experience with the use of pulsatile forces to accelerate treatment. J Clin Orthod. 2015;49(9):557-573.
- Lobre WD, Callegari BJ, Gardner G, Marsh CM, Bush AC, Dunn WJ. Pain control in orthodontics using a micropulse vibration device: A randomized clinical trial. Angle Orthod. 2016; 86(4):625-630.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 David Alpan, DDS, received his Doctor of Dental Surgery degree from Arthur Dugoni School of Dentistry (UOP) and was licensed in California and Nevada in 1996. He earned an Orthodontic Specialty Certificate in 1998 and was awarded a Masters in Science in Dentistry (MSD) for his research on a TMJ project. Dr. Alpan founded his private practices, Alpan Orthodontics, in Los Angeles, Beverly Hills, and Las Vegas in 1999. In 2015, Dr. Alpan transitioned out of the Las Vegas practice and, in 2016, added the Century City location, while merging his Beverly Hills office. He played an integral role for Align Technology Clinical Education Department from 2002-2008 and participated as a consultant and a speaker for 6 years. He was a member of the Ormco Insiders group for 10 years. He is one of the founding members of the Incognito Circle of Excellence and a part of 3M Unitek’s research panel.
David Alpan, DDS, received his Doctor of Dental Surgery degree from Arthur Dugoni School of Dentistry (UOP) and was licensed in California and Nevada in 1996. He earned an Orthodontic Specialty Certificate in 1998 and was awarded a Masters in Science in Dentistry (MSD) for his research on a TMJ project. Dr. Alpan founded his private practices, Alpan Orthodontics, in Los Angeles, Beverly Hills, and Las Vegas in 1999. In 2015, Dr. Alpan transitioned out of the Las Vegas practice and, in 2016, added the Century City location, while merging his Beverly Hills office. He played an integral role for Align Technology Clinical Education Department from 2002-2008 and participated as a consultant and a speaker for 6 years. He was a member of the Ormco Insiders group for 10 years. He is one of the founding members of the Incognito Circle of Excellence and a part of 3M Unitek’s research panel.
