CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This article aims to discuss some ways that early orthodontic treatment can successfully improve and resolve facial asymmetries in young patients.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Realize the importance of diagnosis and treatment of facial asymmetries.
- Identify various etiologies of skeletal asymmetries.
- Recognize important aspects of the clinical exam for proper evaluation of asymmetries.
- Identify the radiographic techniques necessary to determine facial asymmetries.
- Realize the different treatment modalities for distinct types of asymmetries.

Dr. Bradford N. Edgren discusses the importance of diagnosis and treatment of facial asymmetries
Abstract
The most important key to any successful orthodontic treatment is a proper and thorough diagnosis. The same is true for the diagnosis and treatment of facial asymmetries. If a patient’s facial asymmetry is not initially diagnosed, the risk of treatment failure increases, especially in cases with inappropriate/irreversible permanent tooth extraction and/or treatment mechanics. This is especially important in children because facial asymmetries in these young patients generally become more severe with growth and time; therefore, early recognition is imperative. Improper early interceptive orthodontic treatment can accentuate the asymmetry rather than improve it. This includes the underdiagnosis and consequent lack of treatment of upper airway obstructions, enhancing the development and degree of facial asymmetries.1
Introduction
Ideal bodily symmetry in all organisms rarely, if ever exists. Consequently, subtle asymmetries are common in all patients and considered normal. However, the point where the subtle facial asymmetry falls outside the range of normal and becomes aberrant/divergent is not as easily delineated. Often it is the patient’s perception of the lack of facial symmetry, as well as the degree of the imbalance, that determines the necessity and the extent of treatment warranted.2 The investigation of McAvinchey, et al., into the perception of facial asymmetries reported that recognition of an asymmetry was dependent upon the profession of the observer and the severity of the anomaly. Findings of their layperson group classified an asymmetry of 5.6 mm ± 2.7 mm at the chin to be “normal.” They also reported that orthodontists were found to be far more conscious of the presence of an asymmetry than the layperson.3
Treatment of dental asymmetries due to premature deciduous tooth loss, tooth size discrepancies, and/or missing teeth is more easily addressed compared to structural, skeletal asymmetries. Orthodontic treatment techniques to regain space loss, permanent tooth replacement, and asymmetrical extractions are often employed to successfully treat dental asymmetries.
Significant skeletal asymmetries require a combination of orthodontics, dentofacial orthopedics, and possible future orthognathic surgery after the finalization of growth in adolescents. Adults with skeletal anomalies require orthodontics and surgical considerations, unless the patient dictates certain compromises before the initiation of treatment,2 necessitating the importance of informed consent. Even though facial asymmetries can present in Class I malocclusions, they are more often associated with Class II and Class III malocclusions.4 Severt and Proffit reported that clinically apparent facial asymmetries were most often recorded at the level of the chin in 74% of patients, and midface asymmetries were documented in roughly a third (36%). Interestingly, they also noted that when a transverse deviation of the chin occurred, there was a predilection to the left. An exception was with long-faced patients where there was an equal distribution between left and right asymmetries.5
Functional asymmetries, which often result from the mandible deflecting to one side due to maxillary constriction or even a single malpositioned tooth preventing proper intercuspation, can develop into permanent deformities following the cessation of growth. Functional shifts of the occlusion can accentuate or even mask structural asymmetries underscoring the importance of a thorough clinical exam.4 Young patients exhibiting true functional asymmetries can be successfully treated with early interceptive dentofacial orthopedic treatment, including maxillary expansion and orthodontics.
Etiologies of skeletal asymmetries vary and fall into three basic categories, including congenital, environmental, and developmental.4 Congenital and genetic causes of facial asymmetries include cleft lip and palate, hemifacial microsomia, unilateral craniosynostosis6, and zygomaticotemporal synostosis.7
Infection, tumors, and trauma are examples of environmental or acquired etiologies of facial asymmetry. Growth of benign and malignant tumors can distort the dentofacial architecture, misshaping the dentoalveolar arches and jaw bones, resulting in significant facial asymmetries. Early trauma to the temporomandibular joint can result in ankylosis, unilateral condylar hypoplasia, and/or subcondylar fracture, precipitating the onset of facial deformities. Age of onset of an acquired etiology will determine the severity of the asymmetry. Often the earlier the onset, the greater the facial deformity due to growth.
Asymmetries that are developmental in nature are relatively uncommon. Develop-mental asymmetries are non-syndromic, idiopathic, non-congenital, and gradually develop over time, becoming apparent during adolescence.4
Diagnosis and radiographic techniques
A thorough evaluation, including clinical assessment, panoramic imaging, submentovertex radiography, and a complete cephalometric survey with analyses are all important for diagnosis of patients with facial asymmetries. The clinical exam should include an evaluation of dental midlines, Angle classification, open bites, functional shifts, and the presence of anterior and posterior crossbites. Unilateral posterior crossbites can be an indication of a bilateral maxillary constriction with a functional shift to the affected side resulting in a functional asymmetry. A unilateral posterior crossbite can also be indicative of a midface skeletal asymmetry.

Lateral cephalograms, though useful for evaluation of anteroposterior and vertical evaluations of the jaws and dentition relative to the cranial base, are less reliable for assessment of asymmetries. Superimposition of left and right structures as well as magnification errors can mask skeletal asymmetries.4 Posteroanterior radiographs do not result in superimposition or the unequal magnification of the left and right halves of the face and are an important tool in the diagnosis of asymmetries.2 Routine use of the posteroanterior cephalogram and frontal cephalometric analysis can reduce the risk of missing skeletal asymmetries, especially in the young patient who possesses a mild, incipient facial asymmetry that hasn’t been fully expressed because of remaining, future growth.
Submentovertex imaging is another valuable radiographic technique that can be used to assess the shape and symmetry of the inferior border of the mandible, zygomatic arches, and relative position of the condyles. A facial asymmetry that is detected on a posteroanterior cephalogram can be diagnosed as a functional asymmetry when evaluated by the submentovertex radiograph because the left and right inferior borders of the mandible are determined to be symmetrical.
The panoramic radiograph is a convenient image for an initial evaluation of the dentition, maxilla, mandible, pathology, and gross asymmetries. However, it is not as valuable a tool for determination of skeletal asymmetries due to the inherent distortions of this radiographic technique because of patient positioning.8 Observed differences between the left and right halves, unless overt between the temporomandibular joints, ramuses, and the bodies of the mandible, should be interpreted with discretion.
Cone beam computed tomography (CBCT) has neither the magnification errors nor the complications of superimposition of anatomical structures that traditional radiographic techniques possess. Consequently, CBCT imaging is a valuable tool when evaluating facial asymmetry patients.


Patient therapies
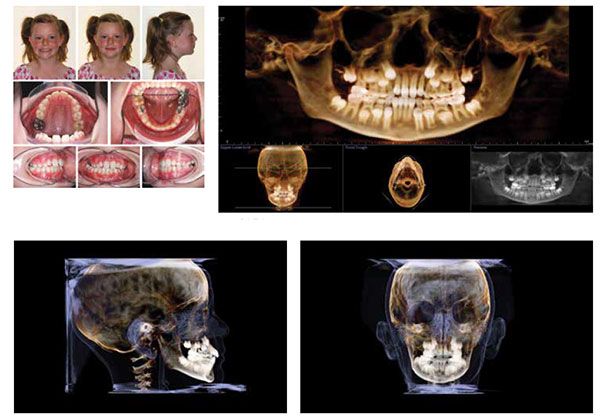
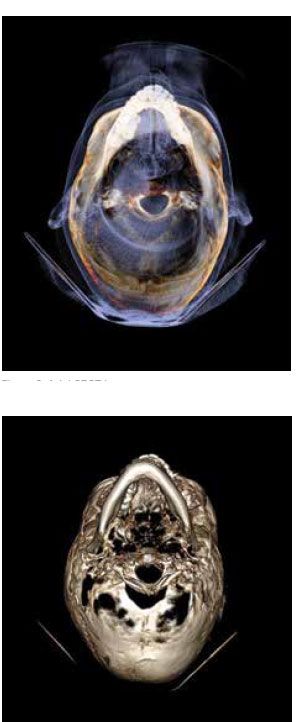
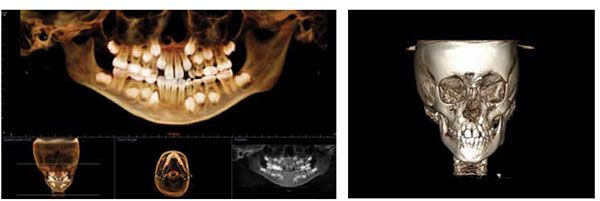
Early interceptive treatment of patients diagnosed with functional asymmetries includes a combination of dentofacial orthopedics and orthodontics. This 8-year 5-month-old female presented with a right functional shift of the mandible resulting in a lower facial asymmetry, posterior crossbite, and a lower dental midline discrepancy of 4.5 mm (Figure 1). Panoramic CBCT imaging reveals dental crowding (Figure 2). The lateral CBCT image shows no evidence of an asymmetry since both lower borders of the mandible are coincident (Figure 3). The frontal CBCT image demonstrates a significant facial asymmetry to the right (Figure 4). Cephalometric analysis of the frontal image revealed a skeletal lingual crossbite pattern due to the maxilla (Figure 5). Axial CBCT images of the patient demonstrate relatively good symmetry of the inferior border of the mandible but with a functional deviation to the right (Figures 6 and 7). The patient was treated with a bonded maxillary expander and orthodontics. Early interceptive treatment time was 31 months. Her maxillary constriction and right posterior crossbite were corrected, and her facial symmetry significantly improved as well (Figures 8, 9, and 10).
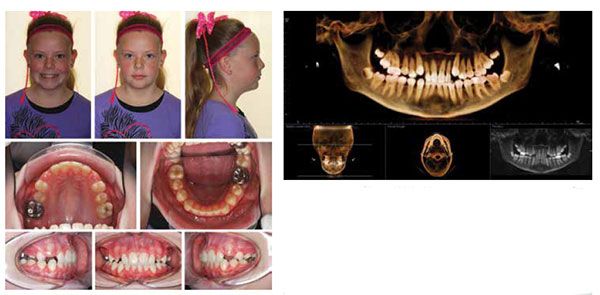
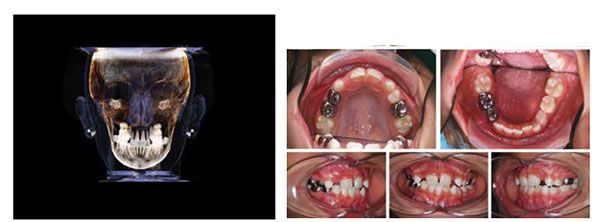
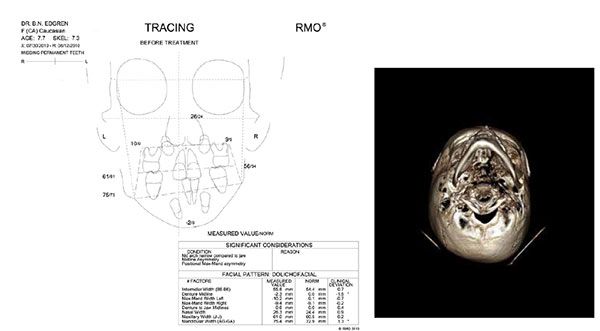
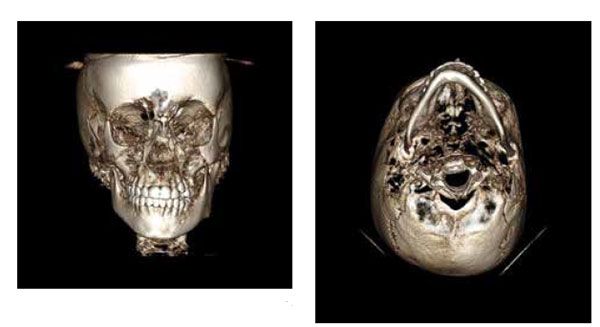
Treatment of patients with structural craniofacial asymmetries is more challenging than those with functional asymmetries. Younger patients can benefit from early interceptive treatment, lessening the severity of a facial asymmetry and therefore reducing the extent of future orthognathic surgery. This 7-year 9-month-old female presented with right-sided hemifacial microsomia (Figure 11). The panoramic CBCT image displays ectopic maxillary lateral incisors and significant crowding (Figure 12). Her frontal volume rendering image discloses a hypoplastic right maxilla and mandible manifesting in significant middle and lower face asymmetries (Figure 13). Frontal cephalometric analysis reveals a notable occlusal cant with the right side superior to the left (Figure 14). The axial image exhibits a misshapen inferior border of the mandible with the right half being notably more underdeveloped than the left (Figure 15).
This young patient’s treatment included maxillary expansion with a bonded expander to stimulate maxillary development and orthodontics. Treatment time was approximately 30 months resulting in a nice Class I occlusion and improvement in her facial asymmetry (Figure 16). Her panoramic image following early interceptive treatment demonstrates acceptable root parallelism and proper eruption of the permanent dentition (Figure 17). Frontal and axial images exhibit improvement in facial asymmetry and lower borders of the mandible (Figures 18 and 19). A boost in self-esteem was an added benefit of early treatment for this patient. The extent of future orthognathic surgery has been reduced, if desired, for this patient.
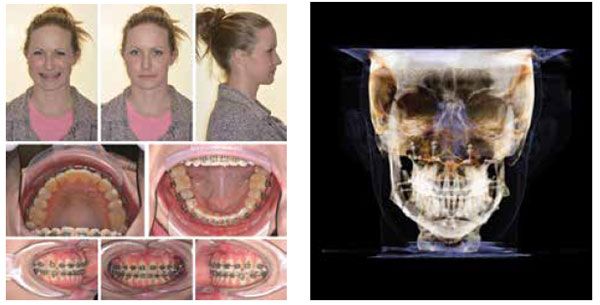
Adult patients generally require a combination of orthodontics and orthognathic surgery to correct significant facial asymmetries. This 27-year 6-month-old adult female fractured her mandible at the age of 5 (Figure 20). At the time, the left subcondylar neck fracture was treated with closed reduction. She suffered from chronic headaches and left jaw joint pain. Intraoral photographs demonstrate a 5 mm lower dental midline deviation to the left, a right-sided Class I malocclusion, and a Class II malocclusion on the left. The panoramic image discloses a complete adult dentition with the exception of the previously extracted third molars (Figure 21). Frontal and axial CBCT images display a significant left-sided facial asymmetry and severely misshapen mandible (Figures 22 and 23). A sectional axial image at the level of the condyles shows a significant alteration in the morphology of the left condyle secondary to the subcondylar fracture at age 5 (Figure 24).
Splint therapy was initially employed to resolve her left temporomandibular joint pain and tension headaches. Following cessation of her joint pain and headaches, the patient was treated with comprehensive ortho-dontics and orthognathic surgery to improve her alignment, stability, and jaw function. Surgical correction included a LeFort I osteotomy, bilateral sagittal split osteotomy, and genioplasty to correct her maxillofacial skeletal and dental anomalies. Post-surgical extraoral and intraoral photos show notable improvement in facial symmetry and dental midline alignment (Figure 25). The post-surgical frontal CBCT image displays significant improvement in her maxillofacial skeleton, especially in mandibular shape and form (Figure 26).
Conclusion
Appropriate early orthodontic treatment can successfully improve and resolve, especially functional, facial asymmetries in young patients. Early treatment requires time to take necessary advantage of growth to be successful. Surgical intervention is sometimes required for these patients as adults; however, the extent of surgical intervention can be reduced with proper early treatment. Adult patients with facial asymmetries require a combination of orthodontics and ortho-gnathics. Careful diagnostic evaluation is essential for successful outcomes.
References
- Edgren BN. Upper airway obstruction – poor function becomes poor form (CE). Orthodontic Practice US. 2013; 4(2):34-37.
- Bishara SE, Burkey PS, Kharouf JG. Dental and facial asymmetries: a review. Angle Orthod. 1994;64(2):89-98.
- McAvinchey G, Maxim F, Nix B, Djordjevic J, Linklater R, Landini G. The perception of facial asymmetry using 3-dimensional simulated images. Angle Orthod. 2014;84(6):957–965.
- Cheong YW, Lo LJ. Facial asymmetry: etiology, evaluation, and management. Chang Gung Med J. 2011;34(4):341–351.
- Severt TR, Proffit WR. The prevalence of facial asymmetry in the dentofacial deformities population at the University of North Carolina. Int J Adult Orthodon Orthognath Surg. 1997;12(3):171-176.
- Arvystas MG, Antonellis P, Justin AF. Progressive facial asymmetry as a result of early closure of the left coronal suture. Am J Orthod. 1985;87(3):240-246.
- Rogers GF, Greene AK, Oh AK, Robson C, Mulliken JB. Zygomaticotemporal synostosis: a rare cause of progressive facial asymmetry. Cleft Palate Craniofac J. 2007;44(1):106-111.
- Rondon RH, Pereira YC, do Nascimento GC. Common positioning errors in panoramic radiography: A review. Imaging Sci Dent. 2014;44(1):1-6.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Bradford N. Edgren, DDS, MS, earned both his Doctorate of Dental Surgery, as Valedictorian, and his Master of Science in Orthodontics from the University of Iowa, College of Dentistry. He is a Diplomate, American Board of Orthodontics, and a member of the Southwest Component of the Edward H. Angle Society. Dr. Edgren has presented nationally and internationally to numerous orthodontic groups on the importance of orthodontic diagnosis, early interceptive orthodontic treatment, CBCT, and upper airway obstruction. He has been published in AJO-DO, the American Journal of Dentistry, as well as other orthodontic publications. Dr. Edgren currently has a private practice in Greeley, Colorado.
Bradford N. Edgren, DDS, MS, earned both his Doctorate of Dental Surgery, as Valedictorian, and his Master of Science in Orthodontics from the University of Iowa, College of Dentistry. He is a Diplomate, American Board of Orthodontics, and a member of the Southwest Component of the Edward H. Angle Society. Dr. Edgren has presented nationally and internationally to numerous orthodontic groups on the importance of orthodontic diagnosis, early interceptive orthodontic treatment, CBCT, and upper airway obstruction. He has been published in AJO-DO, the American Journal of Dentistry, as well as other orthodontic publications. Dr. Edgren currently has a private practice in Greeley, Colorado.
