Editor’s intro: Situational extraction therapy often leads to innovative treatment decisions — these clinicians have discovered that clear aligner therapy can result in a stable, functionally, and esthetically balanced occlusion after atypical extractions.
Drs. George J. Cisneros, Anderson T. Huang, and Darren Huang discuss a case that resulted in a stable, functionally, and esthetically balanced occlusion
Abstract
Complex malocclusions requiring atypical extractions have conventionally been treated with fixed appliances. However, there has been an increasing concern regarding the viability of clear aligner therapy for the treatment of extraction cases. This case report illustrates the treatment with clear aligner therapy of a patient where atypical extractions are required. The patient was a 12-year-old boy with a Class I malocclusion, an ectopically erupted maxillary left canine, dental midline deviation, and proclined maxillary incisors. Our treatment plan involved the exclusive use of clear aligner therapy. We planned for the extraction of the maxillary right first premolar in order to correct the maxillary midline and facilitate the eruption of the maxillary left canine. After 17 months for the initial course of aligners, we prepared adequate space for the maxillary left canine, erupted the maxillary left canine further into the arch, and improved midline coordination. Following a total of 26 months of treatment, in which we performed a single refinement course, we achieved ideal overjet and overbite, proper interdigitation of the maxillary left canine, coordination of maxillary and facial midlines, and Class I canine and molar occlusion bilaterally. Radiographs showed root parallelism between the teeth adjacent to the extraction site. The case report describes the biomechanics behind ClinCheck® (Invisalign®) development for extraction cases treated with clear aligner therapy. We demonstrate that our approach toward extraction therapy produced a stable, functionally, and esthetically balanced occlusion for the patient.
Introduction
Since the introduction of the Invisalign appliance to orthodontics, there has been an increasing interest regarding its use for the successful treatment of complex malocclusions. Early studies described the limitations of Invisalign, including deficiencies in the correction of large anteroposterior discrepancies and occlusal contacts, and unreliability in achieving certain movements, such as bodily translation during space closure, root torque, extrusion, and rotations of premolars and canines.1,2
Nevertheless, recent protocols and innovations in the appliance have allowed for improved adaptability to a wider range of malocclusions. There have been reports of successful treatment with Invisalign in single mandibular incisor extraction cases,3,4,5 symmetrical two or four premolar extraction cases,6,7,8 and cases involving orthognathic surgery complemented with clear aligner therapy.9 A recent randomized clinical trial has shown similar objective grading system scores between Invisalign and fixed appliances in the treatment of Class I adult extraction cases.10
Despite such advances, there remains a great degree of uncertainty regarding the effectiveness of the Invisalign appliance in complex malocclusions, particularly those requiring extractions.11,12,13 Certain extraction patterns, such as unilateral patterns for dental or skeletal asymmetries, require particularly judicious space management and have not been illustrated in previous studies.14 In light of the lack of evidence on Invisalign-treated complex malocclusions in the current literature, we present the following case report to demonstrate the effective management with Invisalign therapy of a case where atypical extractions are indicated.
Diagnosis and treatment plan
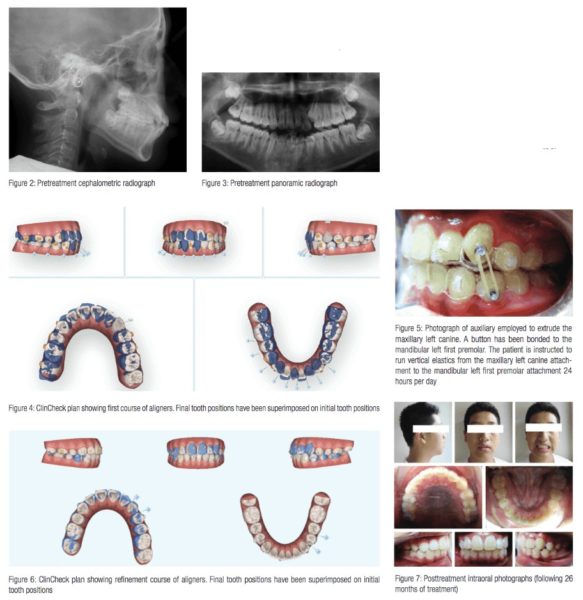
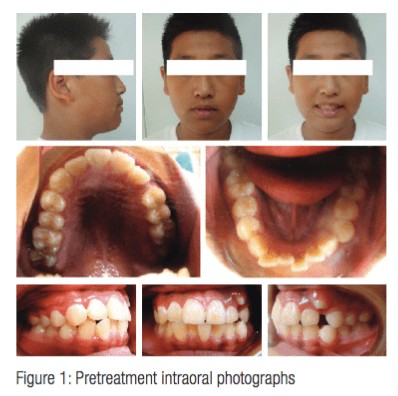 A 12-year-old male presented with Class I malocclusion, Class I molars bilaterally, Class I canine relationship on the right, an unclassifiable canine relationship on the left, shallow overbite, and less than normal overjet (Figure 1). The maxillary arch presented with 6 mm of crowding, while the mandibular arch showed 5 mm of crowding. The maxillary left canine had ectopically erupted, leading to a maxillary midline deviation to the left of about 3 mm. Initial cephalometric analysis showed a Class I skeletal pattern, hyperdivergence, flared maxillary incisors, mandibular incisor inclination within normal range, and less than normal overjet and overbite as shown in Figure 2. The initial panoramic radiograph showed the ectopic eruption of the maxillary left canine and erupting third molars in all four quadrants (Figure 3).
A 12-year-old male presented with Class I malocclusion, Class I molars bilaterally, Class I canine relationship on the right, an unclassifiable canine relationship on the left, shallow overbite, and less than normal overjet (Figure 1). The maxillary arch presented with 6 mm of crowding, while the mandibular arch showed 5 mm of crowding. The maxillary left canine had ectopically erupted, leading to a maxillary midline deviation to the left of about 3 mm. Initial cephalometric analysis showed a Class I skeletal pattern, hyperdivergence, flared maxillary incisors, mandibular incisor inclination within normal range, and less than normal overjet and overbite as shown in Figure 2. The initial panoramic radiograph showed the ectopic eruption of the maxillary left canine and erupting third molars in all four quadrants (Figure 3).
We treatment planned for the extraction of the maxillary right first premolar to facilitate maxillary midline correction and the eruption of the maxillary left canine. We also planned for interproximal reduction in the mandibular arch to allow for decrowding and midline coordination.
Treatment Objectives
Our central treatment objective was to create space for the eruption of the maxillary left canine. Other treatment objectives included coordinating maxillary and mandibular midlines, creating ideal overjet and overbite, correcting maxillary and mandibular crowding, establishing Class I canines, improving maxillary incisor inclination, and creating balanced facial esthetics.
ClinCheck design
Our ClinCheck plan involved an initial course of 35 aligners and a refinement course of 16 additional aligners for a total treatment time of 26 months (Figure 4). We planned for the extraction of the maxillary right first premolar to facilitate the movement of the maxillary midline to the right. We incorporated a gable bend in the extraction space between the maxillary right second premolar and maxillary right canine to optimize root parallelism during space closure. About 1 mm of distalization was planned in the maxillary left segment to create additional space for the maxillary left canine. We requested that the aligners not cover the maxillary left canine, so we could employ auxiliaries to extrude the tooth into the arch during the initial course. In the mandibular arch, we planned for a total of 3 mm of interproximal reduction from the distal of the mandibular right second premolar to the distal of the mandibular left canine. We incorporated a button cutout on the mandibular left first premolar for the future placement of an auxiliary to assist in the extrusion of the maxillary left canine. Class II precision cuts were applied to counteract side effects from distalization on the left side and facilitate maxillary right canine retraction.
During the course of treatment, we bonded metal buttons on the maxillary left canine when there was sufficient crown area and on the mandibular left first premolar, and we instructed the patient to wear vertical elastics full-time to facilitate extrusion of the maxillary left canine (Figure 5).
Treatment progress and refinement
Following the initial course of aligners, the maxillary and mandibular midlines were markedly improved. The space for the maxillary left canine was adequately prepared. However, the maxillary left canine erupted rotated distolabially and required further extrusion for ideal placement into the arch.
In the refinement course, we completed the extrusion of the maxillary left canine and perfected the interdigitation of teeth in the posterior segments (Figure 6). Interproximal reduction was performed mesial and distal to the maxillary left canine and mandibular left first premolar to achieve extrusion of both teeth and ideal interdigitation.
Treatment results
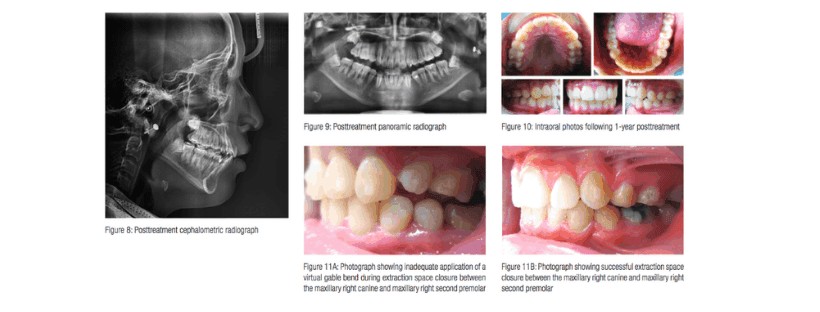
We achieved a final occlusion with Class II molar on the right, Class I molar on the left, and Class I canine relationships bilaterally (Figure 7). The profile was balanced with harmonious soft tissue contours. Both overjet and overbite were ideal. The maxillary left canine was extruded to an esthetically and functionally balanced position and occluded with the mandibular left first premolar. Maxillary and mandibular alignments were close to ideal. The maxillary midline was coincident with the face, while the mandibular midline was 1 mm deviated to the left. Final cephalometric analysis showed that maxillary incisor inclination was normalized, and mandibular incisor inclination was maintained (Figure 8). The panoramic radiograph showed optimal root parallelism between the teeth adjacent to the extraction site (Figure 9).
The retention protocol required the patient to wear maxillary and mandibular Essix retainers 14 hours per day for the first year. At 1 year after debonding, the occlusion showed stability (Figure 10). Maxillary and mandibular alignment were maintained, overbite and overjet were stable, and maxillary and mandibular arch forms were preserved.
 Discussion
Discussion

In the previous case, we achieved our treatment objectives and finished in functionally balanced occlusion. Careful planning during the ClinCheck development stage was critical for the effective closure of all extraction spaces.
We observed that in the case above, we did not receive the G6 maximal anchorage protocol for extraction space closure due to anchorage loss of greater than 2 mm. We note that the ClinCheck plans for extraction cases are frequently disqualified from the G6 maximal anchorage protocol and require the clinician to further design extraction space closure to optimize clinical results. We also recommend the use of a half-sized pontic for the extracted tooth so that the adjacent teeth can receive maximal coverage with the aligner material. In our previous study regarding patients with restorative and prosthodontic needs, we have demonstrated that the design of attachments on the adjacent teeth of extraction spaces is especially important.15 Extraction space closure often requires careful manipulation of tooth movement because the Invisalign appliance has been shown to be less effective at root tipping and at moving roots bodily through bone.10 When the G6 maximal anchorage protocol was not triggered, we employed either conventional vertical beveled attachments or default optimized attachments on the teeth adjacent to the extraction spaces.
In the previous case, we have shown that the addition of a virtual gable bend (VGB) is essential for ideal root parallelism during extraction space closure with clear aligner therapy. In the left figure, the maxillary right canine, maxillary right second premolar, and maxillary right first molar have been reciprocally moved into the maxillary right first premolar extraction space without adequate VGB application (Figure 11A). We can observe the unfavorable tipping of the maxillary right second premolar and maxillary right first molar.
In Figure 11B, the VGB has been applied in the extraction space between the maxillary right canine and maxillary right second premolar during space closure. Ideal root parallelism was achieved, as also demonstrated on the panoramic X-ray (Figure 12).
During ClinCheck development, the VGB allows for the movement of teeth adjacent to extraction spaces in a more practical manner. In particular, the VGB tips then uprights the roots of the adjacent teeth rather than moving them in a random fashion. The addition of the VGB will typically increase the total number of aligners during treatment. We expect an increase of 10-15 aligners in a clear aligner extraction case when the VGB has been incorporated. Nevertheless, we believe its addition significantly improves outcomes in clear aligner extraction therapy.
In their randomized clinical trial, Li, et al., demonstrated that clear aligner therapy could achieve root angulation as successful as fixed appliances in extraction cases.10 The authors postulated that optimal attachment placement contributed to improved root control during treatment.
Midline correction can be sensitive to the development of particular side effects, such as undesired root tipping. In the case previously mentioned, optimized root control attachments were added on the maxillary central incisors to provide for ideal movement of the two roots during midline correction.
The previous case shows an instance where an auxiliary was necessary to supplement a difficult movement for the Invisalign appliance. Historically, extrusion has been demanding, and interarch elastics have been often used as a supplement to achieve ideal occlusal contacts.16 In the presented case, we incorporated a gradually enlarging pontic to simulate the eruption of the maxillary left canine into the arch. The timing for the addition of the auxiliary can be decided on the basis of tracking for the tooth in question. We have observed that significant extrusion — i.e., 3 mm or greater — often requires an additional refinement course to perfect interdigitation.
Total treatment time for the case above was comparable to that which would be necessary had the case been treated with conventional fixed appliances. This result is coincident with the finding of Gu, et al., that on average, Invisalign patients finished 5.7 months faster when compared to matched patients in fixed appliances.17 In refinement courses, we routinely shorten the wear time for each aligner from 2 weeks to 1 week because typically less tooth movement is performed within each aligner.
Conclusion
- In this case report, we have shown that with a combination of meticulous diagnosis and treatment planning along with judicious ClinCheck development, complex extraction cases can be treated to a level of excellence.
- Although G6 technological developments have targeted moderate and maximal extraction cases, atypical extraction cases, such as the case previously mentioned, require innovative measures for the optimization of treatment results.
- We recommend that more randomized clinical trials be performed to gather evidence regarding the viability of clear aligner therapy for extraction cases.
Situational extraction therapy can result in many treatment options, but does the orthodontist’s own experience play a part in determining treatment? See what Drs. Newaz and Jerrold say in their article, “Does having had premolar extractions affect how orthodontists treat their patients? A pilot study.”
- Boyd RL. Esthetic orthodontic treatment using the Invisalign appliance for moderate to complex malocclusions. J Dent Educ. 2008;72(8):948-967.
- Simon M, Keilig L, Schwarze J, Jung BA, Bourauel, C. Treatment outcome and efficacy of an aligner technique — regarding incisor torque, premolar derotation, and molar distalization. BMC Oral Health. 2014;14:68.
- Zawawi, KH. Orthodontic Treatment of a mandibular incisor extraction case with Invisalign. Case Rep Dent. 2014;2014:657.
- Giancotti, A, Garino, F, Mampieri G. Lower incisor extraction treatment with the Invisalign® technique: three case reports. J Orthod. 2015;42(1):33-44.
- Needham R, Waring DT, Malik, OH. Invisalign treatment of Class III malocclusion with lower-incisor extraction. J Clin Orthod. 2015;49(7):429-441.
- Womack, WR. Four-premolar extraction treatment with Invisalign. J Clin Orthod. 2006;40(8):493-500.
- Honn M, Göz, G. A premolar extraction case using the Invisalign system. J Orofac Orthop. 2006;67(5):385-394.
- Giancotti A, Greco M, Mampieri, G. Extraction treatment using Invisalign Technique. Prog Orthod. 2006;7(1):32-43.
- Boyd RL. Surgical-orthodontic treatment of two skeletal Class III patients with Invisalign and fixed appliances. J Clin Orthod. 2005;39(4):245-258.
- Li W, Wang S, Zhang Y. The effectiveness of the Invisalign appliance in extraction cases using the ABO model grading system: a multicenter randomized controlled trial. Int J Clin Exp Med. 2015;8(5):8276-8282.
- Phan X, Ling PH. Clinical limitations of Invisalign. J Can Dent Assoc. 2007;73(3):263-266.
- Lagravere MO, Flores-Mir C. The treatment effects of Invisalign orthodontic aligners: a systematic review. J Am Dent Assoc. 2005;136(2):1724-1729.
- Ko HC, Liu W, Hou D, et al. Recommendations for clear aligner therapy using digital or plaster study casts. Prog Orthod. 2018;19(1):22.
- Djeu G, Shelton C, Maganzini A. Outcome assessment of Invisalign and traditional orthodontic treatment compared with the American Board of Orthodontics objective grading system. Am J. Orthod. Dentofacial Orthop. 2005;28(3):292-298.
- Huang AT, Huang D. Space management with Invisalign for interdisciplinary orthodontic treatment. J Clin Orthod. 2018;52(4):219-226.
- Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. Efficacy of clear aligners in controlling orthodontic tooth movement: a systematic review. Angle Orthod. 2015;85(5):881-889.
- Gu J, Tang JS, Skulski B, et al. Evaluation of Invisalign treatment effectiveness and efficiency compared with conventional fixed appliances using the Peer Assessment Rating index. Am J. Orthod. Dentofacial Orthop. 2017;151(2):259-266.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 George J. Cisneros, DMD, received his dental degree from the University of Pennsylvania School of Dental Medicine and earned specialty certification in both Pediatric Dentistry and Orthodontics, as well as, a Master of Medical Science degree (MMSC) in Oral Biology at Boston’s Children’s Hospital Medical Center, the Forsyth Dental Center, and the Harvard School of Dental Medicine, respectively. Dr. Cisneros developed and established postgraduate training programs in Orthodontics at Albert Einstein College of Medicine/Montefiore Medical Center and Saint Barnabas Hospital in New York, and served as Chair of Orthodontics at New York University College of Dentistry. He is a Diplomate of the American Board of Pediatric Dentistry and the American Board of Orthodontics and has served as an ABO board examiner and on the ABPD Advisory Committee. He also was elected to and served on the American Academy of Pediatric Dentistry Board of Trustees.
George J. Cisneros, DMD, received his dental degree from the University of Pennsylvania School of Dental Medicine and earned specialty certification in both Pediatric Dentistry and Orthodontics, as well as, a Master of Medical Science degree (MMSC) in Oral Biology at Boston’s Children’s Hospital Medical Center, the Forsyth Dental Center, and the Harvard School of Dental Medicine, respectively. Dr. Cisneros developed and established postgraduate training programs in Orthodontics at Albert Einstein College of Medicine/Montefiore Medical Center and Saint Barnabas Hospital in New York, and served as Chair of Orthodontics at New York University College of Dentistry. He is a Diplomate of the American Board of Pediatric Dentistry and the American Board of Orthodontics and has served as an ABO board examiner and on the ABPD Advisory Committee. He also was elected to and served on the American Academy of Pediatric Dentistry Board of Trustees. Anderson T. Huang, BDS, DDS.ABO, FACD, FICD, is a faculty member, Department of Orthodontics, New York University College of Dentistry, New York City, and Department of Orthodontics, Taipei Medical University, Taipei, Taiwan. Dr. Huang is a Diplomate of American Board of Orthodontics (ABO). He is an Invisalign top 1% Platinum Plus provider and treating a wide range of orthodontic cases with clear aligner therapy, including Invisalign®, 3M™ Clarity™ aligners and SureSmile® aligners. He has orthodontic practices in Flushing, Great Neck, and Manhattan, New York. Dr. Anderson Huang was recently appointed as a board examiner of American Board of Orthodontics (ABO).
Anderson T. Huang, BDS, DDS.ABO, FACD, FICD, is a faculty member, Department of Orthodontics, New York University College of Dentistry, New York City, and Department of Orthodontics, Taipei Medical University, Taipei, Taiwan. Dr. Huang is a Diplomate of American Board of Orthodontics (ABO). He is an Invisalign top 1% Platinum Plus provider and treating a wide range of orthodontic cases with clear aligner therapy, including Invisalign®, 3M™ Clarity™ aligners and SureSmile® aligners. He has orthodontic practices in Flushing, Great Neck, and Manhattan, New York. Dr. Anderson Huang was recently appointed as a board examiner of American Board of Orthodontics (ABO). Darren Huang, BS, DDS, is a postgraduate orthodontic resident, New York University College of Dentistry. He will join Dr. Anderson T. Huang’s practices in the summer of 2019. He has co-authored numerous articles with Dr. Anderson Huang during his tenure in the DDS program and postgraduate orthodontic residency.
Darren Huang, BS, DDS, is a postgraduate orthodontic resident, New York University College of Dentistry. He will join Dr. Anderson T. Huang’s practices in the summer of 2019. He has co-authored numerous articles with Dr. Anderson Huang during his tenure in the DDS program and postgraduate orthodontic residency.
