Veteran patient at Cosmetic Dentists of Houston Dr. Lou Shuman discusses how a lifetime of freedom can be repaid by ...
Matt Rej offers tips on how to mitigate the costs of accepting credit cards Credit cards are convenient for patients ...
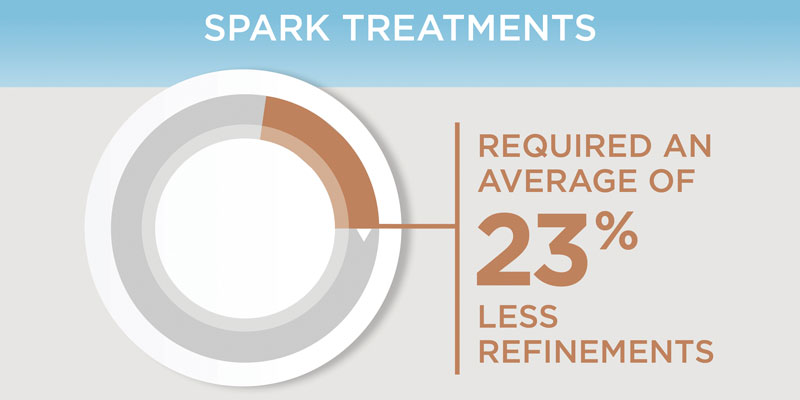
Spark™ Clear Aligner System Spark’s advanced technology enables more sustained force retention and better surface contact with the tooth compared ...
Numerology is the study of numbers that deal with their mystical meaning and effect on our lives. When you think ...
Dr. Neil Warshawsky and Loc X. Phan explore NiTime aligners and their “new generation” of aligner plastic Abstract Although there ...
A better way to manage your new patients from call to close Mary Beth Kirkpatrick, founder of Gaidge and Gaidge ...
Dr. Jane Wright illustrates the clinical and esthetic concerns that drove the treatment plan for this patient Growing up in ...
Dr. Bill Dischinger I’ve worked for over 2 decades as an orthodontist. These have been great years. I was able ...
Protecting your practice from hackers We are all experiencing constant dangerous threats in our digital lives with ongoing attempts to ...
(Left) Dr. Mike Ragan; (Right) DentalMonitoring means seeing your patients every week Dr. Mike Ragan explains how dynamic scheduling helps ...
I’m sitting at my computer on a beautiful day, writing my winter message, and Billy Joel’s song, “Keeping the Faith” ...
Oliver Gelles offers reliable metrics to gauge production and efficiency In today’s challenging economic landscape, marked by factors like inflation ...
Dr. Maria Sokolina discusses a game-changer in long-term stability and sleep apnea treatment Abstract Orthodontic treatments often face challenges related ...
Dr. Gabriela Aurora Asensi discusses treatment of a special needs patient Abstract A case of an unexpectedly found compound odontoma ...
Dr. Brett E. Gilbert and Sue Jeffries discuss the importance of providing a safe space in support of dentists’ mental ...
Drs. Chadwick Augusty, Shadbeh Taghizadeh, Vincent Graves, John Stockstill, and Courtney McCracken (biostatistics) study the perceived association between orthodontics and ...
Drs. Francesca Scilla Smith and Larry W. White discuss centric occlusion, centric relation, and the role of canines Canines Prior ...
Dr. Maria L. Geisinger discusses likely modes of transmission for the virus that causes COVID-19 Aerosols created during dental procedures ...
Editor’s intro: Using combination treatment plans allows Dr. Adam Schulhof to approach appliances like menu options — let him whet your appetite ...
Editor’s intro: Dr. Patrik Zachrisson shows how CEREC Ortho is a very versatile software that has many uses apart from the popular ...
Editor’s Intro: Even Tom Cruise flashes an imperfect smile. Model wide-raging smile esthetics with celebrity photos. Dr. Donald J. Rinchuse discusses ...
Dr. James J. Jasper discusses the efficacy of the Jasper Vektor® Appliance Introduction From the beginning of the modern ortho-dontic ...
Dr. Andrew Wallace uses the principles of “smile design” for a patient seeking cosmetic improvement of his upper and lower ...
Dr. Daniel Klauer uses MFT for his patients on a daily basis for malocclusion and OSA The TMJ & ...
Dr. Jane Wright illustrates the clinical and esthetic concerns that drove the treatment plan for this patient Growing up in ...
Dr. Brigham Stoker illustrates a combination of treatment over 4 years Achieving the bright, confident smile our patients desire can ...
Drs. Jeffrey Miller and Claire Miclat show how CBCT can help an orthodontist plan more strategically Introduction When treating patients ...
Drs. Emad Hussein, Sari Amer, Yazan Ashhab, Khaled Qattawi, Mohammad Abo Mowais, Nezar Watted, Zuhir Anani, and Manal Samarah treat a ...
Dr. Manika Agarwal discusses relying on our strengths to develop a versatile approach The choice The prevalence of social media, ...
Dr. Jeffrey M. Heinz illustrates a clinical case study treated with Spark™ Clear Aligners In my practice, I have traditionally ...
Figure 1: Katelyn Dr. Todd Rankin shares a story of extraordinary teamwork and the stunning transformation of a young woman ...
Dr. Diego Peydro demonstrates treatment for an open bite in seven appointments Introduction Over the years, there have been many ...
Dr. Bill Dischinger illustrates treating a patient’s narrow arches and anterior open bite with clear aligner therapy My orthodontic training ...
Dr. Aron Dellinger discusses treatment with the Roncone PhysioDynamic System (PDS) application of the 20/20 molar bracket Initial impressions utilizing ...
Dr. Bradford Edgren illustrates a patient with dysfunctional remodeling of the condyle A healthy 16-year 10-month-old female presented for a ...
Drs. Todd Bovenizer and Christopher Baker discuss brackets that offered precise control for efficient treatment As we reopen our offices, ...
AUSTIN, April 19, 2024- As a result of the success of their initial partnership, Smile Doctors and DentalMonitoring have announced ...
RICHARDSON, Texas, April 19, 2024 /PRNewswire/ -- KLOwen Orthodontics continues to lead innovation in the orthodontic industry by launching at AAO, ...
We are thrilled to announce that Mary Beth Kirkpatrick, celebrated orthodontic consultant and founder of Gaidge, has been honored with ...
The "Better Way" campaign to showcase how the Invisalign® Palatal Expander System is a more positive patient experience and is ...
Dallas, TX; March 2, 2024 - The Denobi Awards, an industry-wide dental awards program celebrating outstanding individuals and dental teams, ...
Braces On Demand is now integrated with EasyRx®, enabling orthodontic practices to save time and increase productivity through workflow simplification. ...
Quakertown, PA – DEXIS, a leading innovator of dental imaging technologies, is proud to announce IS ScanFlow Quick Connect integration ...
http://orthopracticeus.com/wp-content/uploads/2023/10/DEXassist-Animation.mp4 <Quakertown, PA, October 4, 2023> — Leading innovator of dental imaging technologies, sensors, intraoral scanning, and CBCT solutions, DEXIS ...
Tops DPX Delivers Seamless and Integrated Patient Engagement for Orthodontic Practices Through a Comprehensive Communication Platform Alpharetta, Ga. — October ...
Dallas, TX; September 25, 2023 – The Denobi Awards, an industry-wide dental awards program celebrating outstanding individuals and dental teams, ...
Tech CFO joins LightForce after the announcement of Series D funding. BURLINGTON, MA. (Sept. 2023) - In an exciting development, ...
Brand Commits to Sustainability by Launching Free Recycling Program through TerraCycle TRENTON, N.J., September 20, 2023 – Clear Blue Smiles, the ...
FOLLOW US ONLINE
Useful Links
Subscribe Today
Online Dental CE
Copyright © 2024 Orthodontic Practice US - Dental Journal and Online Dental CE | MedMark LLC
15720 North Greenway Hayden Loop, Suite #9 Scottsdale, AZ 85260 | All rights Reserved | Privacy Policy | Terms & Conditions