Drs. Rohit C.L. Sachdeva, Takao Kubota, and Kazuo Hayashi discuss various factors involved in the
treatment of a midline discrepancy
 Introduction
Introduction
The versatility of using suresmile® in the management of patients presenting with a range of malocclusions, including Class 1, Class 2, Class 3, and open bites and deep bites with or without extraction therapy, has been discussed at length in previous articles.1-16
[userloggedin]
The etiology of midline and transverse related malocclusions is multifactorial, and successful treatment of such patients requires a robust understanding of the factors contributing to the malocclusion (Table 1). Successful treatment outcome requires the design of a plan of care that includes a consistent therapeutic strategy.
Generally speaking, midline and transverse problems commonly manifest concurrently in patients with malocclusions. The aim of this article is to discuss the application of suresmile in managing the total care of such patients.
Patient SI
Patient SI, a 15-year-old female, presented with a Class 1 malocclusion, moderate crowding in the upper and lower arches, and a dental midline discrepancy of 2.5 mm. There were two components to the midline discrepancy. The upper midline was about 1.0 to the left of the patient’s facial midline. This was the result of the skewed upper anterior arch. The lower was about 1.5 mm to the right of the facial midline as a result of a mandibular shift. Interferences resulting from the mesio-lingual rotation of the upper right central incisor appeared to be the trigger point for mandibular displacement (Figure 1).
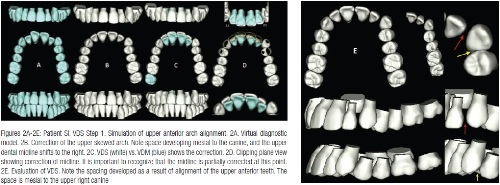
Before initiating treatment, a 3D care plan was designed (Figure 2). The upper facial midline was selected as the treatment midline. The dynamic arch length discrepancy was measured, and it was realized that the patient could be treated non-extraction to a Class 1 occlusion without overtly advancing the incisors or substantially expanding the arches. The plan was formulated through a series of sequential steps. These are briefly described below:
Step 1: Correction of the upper skewed arch
The skewed upper anterior archform was first aligned through asymmetric dental movement of the incisors. This movement helped correct the midline partially by shifting it to the patient’s right. Also, it removed the potential prematurities that caused the mandibular shift and additionally opened up some space on the distal of the upper left canine to facilitate its alignment in the arch (Figure 2).
Step 2: Correction of the upper archwidth
The upper and lower archwidth were evaluated and the bucco-lingual axial inclinations of the buccal segments were evaluated. It was noted that the buccal segments were tipped lingually (Figure 3). The upper archwidth was corrected by a combination of translation and tipping movements (Figure 4). This resulted in the gain of additional space on the distal side of the upper canine, which would help in the alignment of the canine, (Figure 4A).
Step 3: Correction of the mandibular shift and residual midline discrepancy
Mandibular movement was simulated to correct its displacement by shifting it to the patient’s left. The virtual diagnostic simulation (VDS) is shown in Figure 5.
Step 4: Alignment of the lower anteriors and lower archwidth
The lower anterior teeth were aligned as well as the lower buccal segment uprighted (Figure 6).
Step 5: Alignment of the upper canine, establishing the level of the esthetic occlusal plane and detailing the occlusion
The VDS is shown in Figure 7A. The upper left canine was extruded into the space created by the correction of the skewed anterior arch and expansion of the buccal segment (Figures 7B and 7C). The maxillary functional occlusal plane was selected as the treatment occlusal plane. To this treatment plane, the upper anterior occlusal plane was extruded (Figure 8). A comparison of the VDS versus VDM with the associated displacement values of the dentition is shown in (Figure 8). Table 2 summarizes the main steps in designing the VDS for patient SI.
As one may see, performing a VDS, which is an integral part of the practice of BioDigital Orthodontics, provides a host of benefits to both the doctor and the patient. These include the ability to plan and visualize care in 3D, anticipate potential risks, design mechanics (since the nature of planned tooth movement is visualized and can be measured), establish patient decision aids, and manage the care of a patient by defining care milestones based upon the anticipated response (Sachdeva).
 Once the treatment plan was designed, the upper arch was bonded (Tomy CLIPPY-C, aka, In-Ovation® C by Dentsply GAC International bracket with a slot width of .0180″). Treatment was initiated in the upper arch to correct the skewed arch. A slightly expanded .016″ CuNiTi AF 35ºC wire was installed. The upper left canine was engaged as it was recognized that alignment of the upper anterior arch and expansion of the buccal segments would create sufficient space for the alignment of the canine. The risk of a cant developing in the anterior occlusal plane was considerably reduced since the constraints limiting the extrusion of the canine into the arch were assessed to be minimal (Figure 9A). Upper arch alignment was achieved in 8 weeks’ time. As predicted, an anterior cant did not develop. Also, the upper archwidth was substantially corrected. And, the upper midline was partially corrected as per plan. At this appointment, an upper utility arch was placed to help jump the bite and lower arch expansion initiated (Figure 9B). Four months into treatment, positive overjet and lower buccal segment archwidth were established. The upper and lower buccal archwidths were established. Note the mandible has shifted to the right, and the upper and lower midlines are coincident. A .016″ CuNiTi AF 35ºC was inserted to initiate alignment in the lower arch. (Figure 9C). Two months later, the lower anterior segment was aligned. Rectangular .017″ x .025″ CuNiTi AF 35ºC archwires were installed in both the upper and lower arches and light box elastics applied in the buccal segment to help settle it down (Figure 9D).
Once the treatment plan was designed, the upper arch was bonded (Tomy CLIPPY-C, aka, In-Ovation® C by Dentsply GAC International bracket with a slot width of .0180″). Treatment was initiated in the upper arch to correct the skewed arch. A slightly expanded .016″ CuNiTi AF 35ºC wire was installed. The upper left canine was engaged as it was recognized that alignment of the upper anterior arch and expansion of the buccal segments would create sufficient space for the alignment of the canine. The risk of a cant developing in the anterior occlusal plane was considerably reduced since the constraints limiting the extrusion of the canine into the arch were assessed to be minimal (Figure 9A). Upper arch alignment was achieved in 8 weeks’ time. As predicted, an anterior cant did not develop. Also, the upper archwidth was substantially corrected. And, the upper midline was partially corrected as per plan. At this appointment, an upper utility arch was placed to help jump the bite and lower arch expansion initiated (Figure 9B). Four months into treatment, positive overjet and lower buccal segment archwidth were established. The upper and lower buccal archwidths were established. Note the mandible has shifted to the right, and the upper and lower midlines are coincident. A .016″ CuNiTi AF 35ºC was inserted to initiate alignment in the lower arch. (Figure 9C). Two months later, the lower anterior segment was aligned. Rectangular .017″ x .025″ CuNiTi AF 35ºC archwires were installed in both the upper and lower arches and light box elastics applied in the buccal segment to help settle it down (Figure 9D).
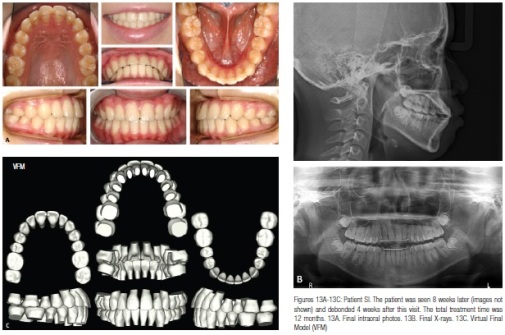
A therapeutic scan was taken 6 weeks later (7.5 months from start of active treatment) (Figure 10).
A virtual target setup and .017″ x .025″ CuNiTi suresmile precision archwires were designed (Figure 11). The suresmile precision archwires were placed 1.5 months post therapeutic scan (Figure 12). The patient progress was evaluated 8 weeks later. The patient was debonded 4 weeks later. The final records are shown in Figure 13. The total treatment time was 12 months. Also, the superimposition of the VDS with the VFM shows that the treatment objectives were met (Figure 14)
Patient TS
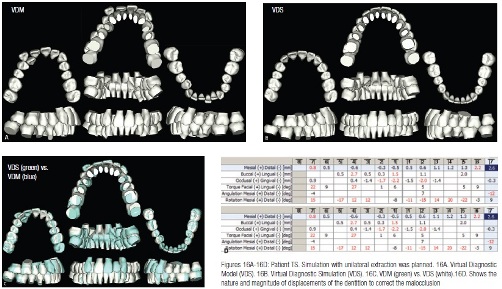
 Patient TS, a 20-year-old female, presented with a Class 2 subdivision right malocclusion. The upper arch demonstrated severe arch length deficiency with a completely blocked-out upper right lateral incisor. The upper midline was shifted to the right of the patient’s facial midline as a result of the tipping of the upper incisors toward the blocked tooth. The lower arch demonstrated moderate crowding (Figure 15). Based upon a dynamic arch length discrepancy analysis (Sachdeva), it was decided to treat the patient with a unilateral extraction of the upper right buccally erupted canine. The facial midline was selected as the treatment midline, and the treated occlusion would be Class 2 occlusion on the right and Class 1 on the left. The VDS is shown in Figure 16.
Patient TS, a 20-year-old female, presented with a Class 2 subdivision right malocclusion. The upper arch demonstrated severe arch length deficiency with a completely blocked-out upper right lateral incisor. The upper midline was shifted to the right of the patient’s facial midline as a result of the tipping of the upper incisors toward the blocked tooth. The lower arch demonstrated moderate crowding (Figure 15). Based upon a dynamic arch length discrepancy analysis (Sachdeva), it was decided to treat the patient with a unilateral extraction of the upper right buccally erupted canine. The facial midline was selected as the treatment midline, and the treated occlusion would be Class 2 occlusion on the right and Class 1 on the left. The VDS is shown in Figure 16.
The upper arch was bonded (Tomy CLIPPY-C, aka, In-Ovation C by Dentsply GAC International bracket with a slot width of .0180″) and to achieve anterior alignment in the upper arch, a .016″ x .022″ CuNiTi AF 35°C archwire was installed. A slightly active open coil spring was placed between the upper right first bicuspid and upper right central incisor to help shift the upper midline to the left by tipping the incisors as well as to correct the skew in the upper arch. This also created some additional space to bring the upper right lateral into the arch (Figure 17A). The patient was next seen 6 weeks later, and at this time, the upper right lateral was bonded and engaged into the archwire. To facilitate the engagement of the lateral incisor, the upper rectangular archwire was replaced with a .016″ CuNiTi AF 35°C archwire (Figure 17C). 1.5 months later, the lower arch was bonded, and a .016″ CuNiTi AF 35°C alignment archwire engaged (Figure 17D). Six months from the start of treatment, the round upper archwire was replaced with a .016″ x .022″ CuNiTi AF 35°C to provide additional stiffness to correct the upper anterior archform (Figure 17E).
The next progress appointment was scheduled 6 weeks later. At this time, a therapeutic scan was taken. Note the upper arch form has improved in its symmetry. Furthermore, the upper lateral incisor has now been brought into the arch, and the lower arch is aligned. The therapeutic scan is shown in Figure 18. The virtual target setup and .017″ x .025″ CuNiTi suresmile precision archwires were designed (Figure 19).
The precision archwires were inserted 6 weeks post therapeutic scan (Figure 20A). The patient was seen 8 weeks later (Figure 20B). At this stage of treatment, it was decided that the patient would be ready for debonding in 4 weeks’ time. Final records at debonding were taken (Figure 21). The superimposition of the virtual diagnostic simulation (VDS) on the virtual final model (VFM) shows that the treatment goals were met (Figure 22). The active treatment for the patient was 12 months.
Discussion/Conclusions
Correction of a patient’s midline discrepancy requires a comprehensive understanding of the nature of the problem, an objective-driven plan, and the implementation of a therapeutic strategy that complements the plan. Breakdown in any of these elements may affect patient care adversely.
Designing a plan of care with the aid of simulations requires expertise and is a skill that a clinician needs to develop. Simulations have little or no value if they do not encompass realistic expectations that are driven by a clinician’s understanding of the nature of tooth displacement in response to applied forces. 3D simulation-guided plans provide an invaluable resource to establish visual clarity of a treatment plan, helps the doctor measure personal performance, and are an excellent patient communication aid.
Acknowledgments
The authors express their sincerest thanks both to Sharan Aranha BDS, MPA, and Arjun Sachdeva for their tireless efforts in the preparation of this article.
References
1. White L, Sachdeva R. Transforming orthodontics: Part 1 of a conversation with Dr. Rohit Sachdeva, co-founder and chief clinical officer of Orametrix Inc. by Dr. Larry White. Orthodontic Practice US. 2012;3(1):10-14.
2. White L, Sachdeva R. Transforming orthodontics: Part 2 of a conversation with Dr. Rohit Sachdeva, co-founder and chief clinical officer of Orametrix Inc. by Dr. Larry White. Orthodontic Practice US. 2012;3(2):6-10.
3. White L, Sachdeva R. Transforming orthodontics: Part 3 of a conversation with Dr. Rohit Sachdeva, co-founder and chief clinical officer of Orametrix Inc. by Dr. Larry White. Orthodontic Practice US. 2012;3(3):6-9.
4. Sachdeva R. BioDigital orthodontics: Planning care with suresmile technology: Part 1. Orthodontic Practice US. 2013;4(1):18-23.
5. Sachdeva R. BioDigital orthodontics: Designing customized therapeutics and managing patient treatment with suresmile technology: Part 2. Orthodontic Practice US. 2013;4(2):18-26.
6. Sachdeva R. BioDigital Orthodontics: Diagnopeutics with suresmile technology (Part 3). Orthodontic Practice US. 2013;4(3):22-30.
7. Sachdeva R. BioDigital orthodontics: Outcome evaluation with suresmile technology: Part 4. Orthodontic Practice US. 2013;4(4):28-33.
8. Sachdeva R. BioDigital orthodontics. Management of Class 1 non–extraction patient with “Fast–Track”©– six month protocol: Part 5. Orthodontic Practice US. 2013;4(5):18-27.
9. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Management of Class 1 non–extraction patient with “Standard–Track”©– nine month protocol: Part 6. Orthodontic Practice US. 2013;4(6):16-26.
10. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Management of space closure in Class I extraction patients with suresmile: Part 7. Orthodontic Practice US. 2014;5(1):14-23.
11. Sachdeva R, Kubota T, Moravec S. BioDigital orthodontics. Part 1-Management of Class 2 non–extraction patients: Part 8. Orthodontic Practice US. 2014;5(2):11-16.
12. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Part 2-Management of patient with Class 2 malocclusion non–extraction: Part 9. Orthodontic Practice US. 2014;5(3):29-41.
13. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Part 3- Management of patients with Class 2 malocclusion extraction: Part 10. Orthodontic Practice US. 2014;5(4):27-36.
14. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Management of patients with class 3 malocclusion: Part 11. Orthodontic Practice US. 2014;5(5):28-38.
15. Sachdeva RCL, Kubota T. BioDigital orthodontics. Part 1 – Management of patients with openbite: Part 12. Orthodontic Practice. 2014;5(6):22-31.
16. Sachdeva RCL, Kubota T,Lohse.J. BioDigital orthodontics. Part 2- Management of patients with openbite: Part 13. Orthodontic Practice 2015;6(1):13-23.
17. Proffit W, Turvey T. Dentofacial asymmetry. In: WR Proffit, RP White, DM Sarver, eds. Contemporary Treatment of Dentofacial Deformity. St. Louis, MO: Mosby; 2003.
18. Burstone CJ. Diagnosis and treatment planning ofpatients with asymmetries. Paper presented at: Seminars in Orthodontics; 1998.
19. Chia MSY, Naini FB, Gill DS. The Aetiology, Diagnosis and Management of Mandibular Asymmetry. Ortho Update 2008;1:44-52.
20. Buranastidporn B, Hisano M, Soma K. Articular disc displacement in mandibular asymmetry patients. J Med Dent Sci. 2004;51(1):75-81.
21. Dong Y, Wang XM, Wang MQ, Widmalm SE. Asymmetric muscle function in patients with developmental mandibular asymmetry. J Oral Rehabil. 2008;35(1):27-36.
22. Kebede B, Megersa S. Idiopathic masseter muscle hypertrophy. Ethiop J Health Sci. 2011;21(3):209-212.
23. Minich CM. An evaluation of skeletal and dental asymmetries in Class II subdivision malocclusions using cone-beam computed tomography. [abstract]. Saint Louis University: 2011.
24. Doyle WJ, Johnston O. On the meaning of increased fluctuating dental asymmetry: a cross populational study. Am J Phys Anthropol. 1977;46(1):127-134.
25. Pinho S, Ciriaco C, Faber J, Lenza MA. Impact of dental asymmetries on the perception of smile esthetics. Am J Orthod Dentofacial Orthop. 2007;132(6):748-753.
[/userloggedin]
[userloggedout][/userloggedout]
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores